TRIAL DESIGN AND OVERSIGHT
We are conducting this ongoing, 2-year, multicenter, randomized, double-blind, placebo-controlled, phase 3, pivotal trial in Argentina, Brazil, Chile, Colombia, Mexico, Peru, South Africa, and the United States. All the participants provided written informed consent. The trial adheres to the principles of the Declaration of Helsinki and to the Good Clinical Practice guidelines of the International Council for Harmonisation. The protocol (available with the full text of this article at NEJM.org) and amendments were approved by institutional review boards according to local regulations. An unblinded independent data and safety monitoring board continuously monitors safety, including monitoring for vaccine-associated enhanced respiratory disease.
The trial is a collaboration between the sponsor, Janssen Research and Development, which is an affiliate of Janssen Vaccines and Prevention and part of the Janssen pharmaceutical companies of Johnson & Johnson, and the Operation Warp Speed Covid-19 Rapid Response Team (which includes the Biomedical Advanced Research and Development Authority, the National Institutes of Health, the Covid-19 Prevention Trials Network, and the Department of Defense). The trial was designed and conducted, and the data analysis and data interpretation were performed, by the sponsor and collaborators. Trial-site investigators collected and contributed to the interpretation of the data. All the data were available to the authors, who vouch for the accuracy and completeness of the data and for the fidelity of the trial to the protocol. Medical writers who were funded by the sponsor assisted in drafting the manuscript.
TRIAL PARTICIPANTS
Stages 1a and 2a of the trial were conducted in parallel and included 2000 adults 18 to 59 years of age and 60 years of age or older, respectively, who were in good or stable health and did not have coexisting conditions that have been associated with an increased risk of severe Covid-19. After a 3-day safety review by the data and safety monitoring board, stages 1b and 2b were initiated. Those stages additionally included adults of the same respective age ranges who had stable and well-controlled coexisting conditions. The eligibility criteria are provided in the Supplementary Methods section in the Supplementary Appendix, available at NEJM.org. Participants were not excluded on the basis of SARS-CoV-2 infection or serostatus.
PROCEDURES
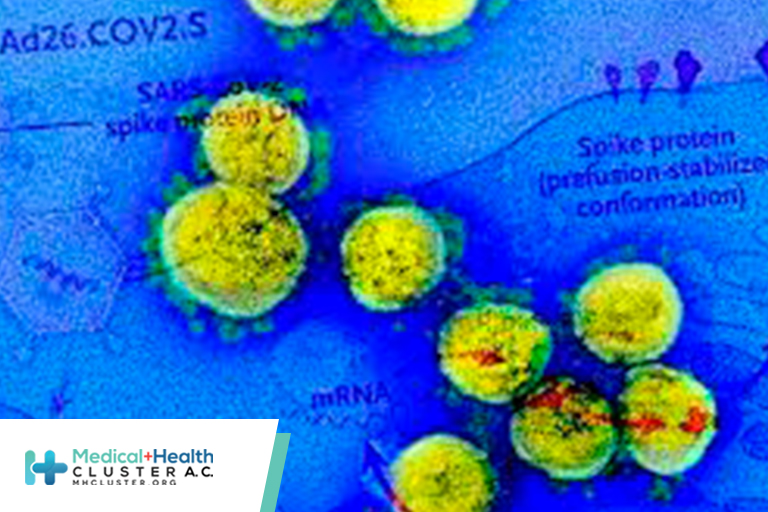
Details of the trial procedures are provided in the Supplementary Methods section. Participants were randomly assigned in a 1:1 ratio, with the use of randomly permuted blocks, to receive either Ad26.COV2.S or saline placebo. Randomization was conducted with an interactive Web-response system and stratified according to trial site, age group, and the presence or absence of coexisting conditions that have been associated with an increased risk of severe Covid-19.
Vaccine or placebo was administered on day 1. Ad26.COV2.S was supplied in single-use vials at a concentration of 1×1011 viral particles per milliliter and was administered at a dose of 5×1010 viral particles as a single intramuscular injection (0.5 ml) by a health care worker who was unaware of the group assignment.
Participants reported Covid-19 symptoms electronically using the Symptoms of Infection with Coronavirus-19 questionnaire (methods described in Fig. S1 in the Supplementary Appendix). Participants and trial staff obtained nasal swabs, which were tested with the use of a Food and Drug Administration (FDA) Emergency Use Authorization reverse-transcriptase–polymerase-chain-reaction (RT-PCR) assay for SARS-CoV-2 at a local laboratory and subsequently confirmed centrally (m-2000 SARS-CoV-2 real-time RT-PCR, Abbott). Seropositivity for SARS-CoV-2 was evaluated by means of a SARS-CoV-2 nucleocapsid (N) immunoassay (Elecsys, Roche) at trial entry and on days 29 and 71. Assays were performed according to the manufacturers’ protocols.
Primary and key secondary efficacy evaluations were based on centrally confirmed cases of Covid-19. Owing to the high incidence of Covid-19 and the time taken for central confirmation, not all cases had been centrally confirmed at the time of the primary analysis. A supplementary analysis of RT-PCR–positive cases from all sources, whether centrally confirmed or not, was therefore performed for subgroups, hospitalizations, and deaths.
SAFETY ASSESSMENTS
Serious adverse events and adverse events leading to withdrawal from the trial are being recorded throughout the trial. In a safety subpopulation comprising approximately 6000 participants (see below), data on solicited local and systemic adverse events were recorded in an electronic diary for 7 days after administration and unsolicited adverse events for 28 days after administration.
EFFICACY ASSESSMENTS
The two primary end points were the efficacy of the Ad26.COV2.S vaccine against the first occurrence of centrally confirmed moderate to severe–critical Covid-19 with an onset at least 14 days after administration and at least 28 days after administration in the per-protocol population (see below). All the potential cases of severe–critical Covid-19 and cases of moderate Covid-19 with at least three signs or symptoms were classified as being severe–critical by an independent Clinical Severity Adjudication Committee whose members were unaware of the group assignments. This committee adjudicated cases on the basis of clinical judgment (e.g., a single low oxygen-saturation measurement was not classified as indicating severe Covid-19 unless other clinical findings were consistent with a severe classification). The case definitions for Covid-19 and the protocol-defined secondary and exploratory end points are described in the Supplementary Appendix.
STATISTICAL ANALYSIS
The full analysis set included all the participants who underwent randomization and received a dose of trial vaccine or placebo. The per-protocol population comprised participants who received a dose of trial vaccine or placebo, were seronegative or had an unknown serostatus at the time that the vaccine or placebo was administered, and had no protocol deviations that were likely to affect vaccine efficacy. Participants who were RT-PCR–positive between days 1 and 14 or between days 1 and 28 were excluded from the analysis of cases with an onset at least 14 days after administration and at least 28 days after administration, respectively. The per-protocol population was the main population for the efficacy analyses. Safety analyses were conducted in the full analysis set, including the safety subpopulation.
The null hypothesis was that the efficacy of Ad26.COV2.S would be no higher than 30% for each primary end point, as evaluated with a truncated sequential probability ratio test15,16 at a one-sided significance level of 0.025. The sample size was reduced from 60,000 to approximately 40,000 on the basis of the high incidence of Covid-19 during the trial. The primary analysis was triggered on a positive recommendation from the data and safety monitoring board, after the FDA-specified median 8-week follow-up was reached and prespecified data requirements were met.
If the null hypothesis was rejected for both primary end points, secondary objectives were evaluated against a null hypothesis that used a lower limit of vaccine efficacy of more than 0% with prespecified multiplicity adjustments for familywise type I error control (Fig. S2). Exact Poisson regression17 was used for the analysis of vaccine efficacy and the associated confidence interval calculations, with accounting for follow-up time. The cumulative incidence over time was estimated with the use of Kaplan–Meier methods to evaluate the onset of vaccine efficacy and vaccine efficacy over time. Participants had their data censored at the end of their follow-up.
The frequency of serious adverse events was tabulated in the full analysis set. The frequency and severity of solicited and unsolicited adverse events were tabulated in the safety subpopulation.