En atención a la creciente preocupación sobre la confianza en...
Leer más
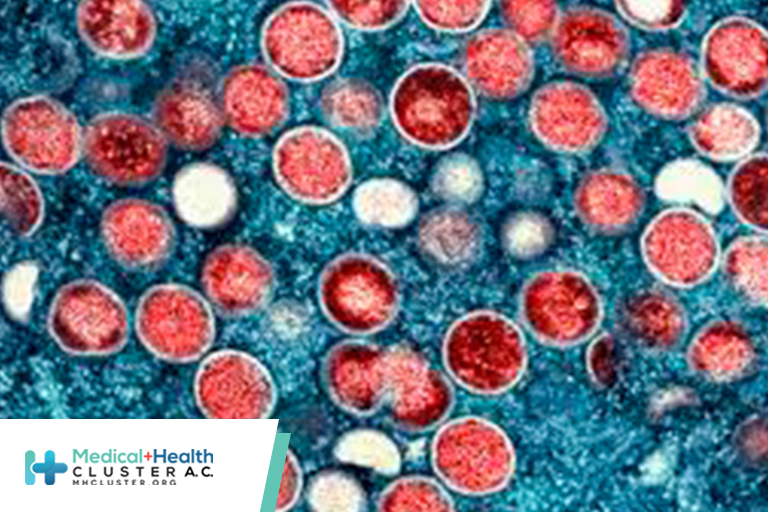
HIV and Sexually Transmitted Infections Among Persons with Monkeypox
Summary
What is already known about this topic?
In the current global monkeypox outbreak, HIV infection and sexually transmitted infections (STIs) are highly prevalent among persons with monkeypox.
What is added by this report?
Among 1,969 persons with monkeypox in eight U.S. jurisdictions, 38% had HIV infection, and 41% had an STI in the preceding year. Among persons with monkeypox, hospitalization was more common among persons with HIV infection than persons without HIV infection.
What are the implications for public health practice?
It is important to leverage systems for delivering HIV and STI care and prevention and prioritize persons with HIV infection and STIs for vaccination. Screening for HIV and other STIs and other preventive care should be considered for persons evaluated for monkeypox, with HIV care and HIV preexposure prophylaxis offered to eligible persons.
High prevalences of HIV and other sexually transmitted infections (STIs) have been reported in the current global monkeypox outbreak, which has affected primarily gay, bisexual, and other men who have sex with men (MSM) (1–5). In previous monkeypox outbreaks in Nigeria, concurrent HIV infection was associated with poor monkeypox clinical outcomes (6,7). Monkeypox, HIV, and STI surveillance data from eight U.S. jurisdictions* were matched and analyzed to examine HIV and STI diagnoses among persons with monkeypox and assess differences in monkeypox clinical features according to HIV infection status. Among 1,969 persons with monkeypox during May 17–July 22, 2022, HIV prevalence was 38%, and 41% had received a diagnosis of one or more other reportable STIs in the preceding year. Among persons with monkeypox and diagnosed HIV infection, 94% had received HIV care in the preceding year, and 82% had an HIV viral load of <200 copies/mL, indicating HIV viral suppression. Compared with persons without HIV infection, a higher proportion of persons with HIV infection were hospitalized (8% versus 3%). Persons with HIV infection or STIs are disproportionately represented among persons with monkeypox. It is important that public health officials leverage systems for delivering HIV and STI care and prevention to reduce monkeypox incidence in this population. Consideration should be given to prioritizing persons with HIV infection and STIs for vaccination against monkeypox. HIV and STI screening and other recommended preventive care should be routinely offered to persons evaluated for monkeypox, with linkage to HIV care or HIV preexposure prophylaxis (PrEP) as appropriate.
Eight health departments matched probable and confirmed cases of monkeypox† diagnosed through July 22, 2022, and occurring among persons aged ≥18 years, to local HIV and STI surveillance data using individually established methods that included various personal identifiers (e.g., name, soundex,§ date of birth, address, and telephone number). Matched data were deidentified and securely transmitted to CDC for analysis.
Among persons with monkeypox, prevalence of diagnosed HIV infection, determined through local HIV surveillance matches,¶ was calculated. HIV surveillance data were used to assess receipt of HIV care,** HIV viral suppression (an indication of antiretroviral therapy use),†† most recent CD4 count,§§ and time since HIV diagnosis (8). STI surveillance data were used to assess chlamydia, gonorrhea, and syphilis diagnoses. Monkeypox signs, symptoms, and outcomes were compared according to HIV infection status. This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy.¶¶
Among 1,969 persons aged ≥18 years with monkeypox diagnosed during May 17–July 22, 2022, in eight participating jurisdictions, 755 (38%) had received an HIV diagnosis, 816 (41%) had another reportable STI diagnosed in the preceding year, and 363 (18%) had both; 1,208 (61%) persons had either (Table 1) (Table 2).*** Since May 1, 2022, 19 (1%) persons with monkeypox had received an HIV diagnosis, and 297 (15%) had received an STI diagnosis. Persons with monkeypox and HIV infection more commonly had received an STI diagnosis in the preceding year (48%) than had those without HIV infection (37%).
Among persons with monkeypox, the weekly percentage with concurrent HIV infection increased over time (31%–44% by July). The percentage of persons with monkeypox who had HIV infection was higher in older age groups: among persons aged 18–24 years, HIV prevalence was 21%, and among those aged ≥55 years, was 59%. HIV prevalence among persons with monkeypox also varied by race and ethnicity, ranging from a high of 63% among non-Hispanic Black or African American (Black) persons, to 41% among Hispanic or Latino (Hispanic) persons, 28% among non-Hispanic White persons, and 22% among non-Hispanic Asian persons.
Among 755 persons with monkeypox and HIV infection, 713 (94%) received HIV care in the preceding year, 618 (82%) were virally suppressed, and 586 (78%) had CD4 count ≥350/μL. The median interval since HIV diagnosis was 10 years (IQR = 6–15 years). Data on HIV PrEP use were available for 172 (14%) persons without HIV infection, 115 (67%) of whom reported current PrEP use.
Compared with persons with monkeypox who did not have HIV infection, those with HIV infection were more likely to report rectal pain (34% versus 26%), tenesmus (20% versus 12%), rectal bleeding (19% versus 12%), purulent or bloody stools (15% versus 8%), and proctitis (13% versus 7%), but were less likely to report lymphadenopathy (48% versus 53%) (Figure). The prevalence of other signs and symptoms was similar among persons with monkeypox with and without HIV infection. Among 564 persons with monkeypox, HIV, known HIV viral load values, and signs and symptoms data, the 51 persons with unsuppressed HIV viral load were more likely than were the 513 with suppressed viral load to have lymphadenopathy (59% versus 46%), generalized pruritis (59% versus 42%), rectal bleeding (25% versus 18%), and purulent or bloody stools (22% versus 14%). Compared with persons with CD4 counts ≥350/μL, those with CD4 counts <350/μL more commonly experienced fever (69% versus 59%) and generalized pruritis (53% versus 42%).
Among 1,308 (66%) persons with information on hospitalization, the proportion of persons hospitalized with monkeypox was lower among those without HIV infection (3%, 26 of 798) than among those with HIV infection (8%, 42 of 510). Among 45 persons with monkeypox and HIV infection who were not virally suppressed, 12 (27%) were hospitalized, and among 61 with a CD4 count <350 cells/μL, nine (15%) were hospitalized.
Top
Discussion
Among persons with monkeypox in eight U.S. jurisdictions, prevalences of concurrent HIV infection and reportable STI diagnoses within the preceding 12 months were high, consistent with previous reports (1–5). To date, most U.S. monkeypox cases have occurred among MSM (4), who have higher prevalences of HIV infection and STIs than the general population. However, in this analysis, the percentage of persons with monkeypox who had HIV infection (38%) was higher than national HIV prevalence estimates for U.S. MSM (23%); this finding was also true when comparing Monkeypox virus and HIV coinfection among Black persons (63%), Hispanic persons (41%), and persons aged ≥55 years (59%) to overall HIV prevalences among Black MSM (39%), Hispanic MSM (19%), and MSM aged 50–60 years (32%), respectively (9). Increasing HIV prevalence among persons with monkeypox over time suggests that monkeypox might be increasingly transmitted among networks of persons with HIV infection, underscoring the importance of leveraging HIV and STI care and prevention delivery systems for monkeypox vaccination and prevention efforts.††† Consideration should be given to prioritizing persons with HIV infection and STIs for vaccination and other prevention efforts. HIV and STI screening and other recommended preventive care§§§ should be routinely offered to persons evaluated for monkeypox, with linkage to HIV care or HIV PrEP, as appropriate.
The proportion of persons with Monkeypox virus and HIV coinfection who received HIV care (94%) exceeded the overall percentage of persons with diagnosed HIV infection who received care in 2020 (74%) (8). Approximately two thirds of persons with monkeypox without HIV infection for whom data were available reported HIV PrEP use, whereas nationally, an estimated 25% of eligible persons received an HIV PrEP prescription in 2020 (8). Moreover, 41% of persons with monkeypox had received a diagnosis of another reportable STI in the preceding year. These findings suggest that reported monkeypox cases are occurring among persons with recent access to HIV and sexual health services. Referral bias might partially explain these findings, as persons with monkeypox signs and symptoms who have established connections with HIV or sexual health providers might be more likely to seek care (2), and these providers might be more likely to recognize and test for Monkeypox virus. Monkeypox signs and symptoms might have led persons with HIV infection who have not been in HIV care to reengage in care. Persons with monkeypox signs and symptoms who are not engaged in routine HIV or sexual health care, or who experience milder signs and symptoms, might be less likely to have their Monkeypox virus infection diagnosed. To ensure appropriate diagnosis and treatment, it is important that health care providers who do not specialize in HIV or sexual health become familiar with the clinical guidance for monkeypox diagnosis and treatment.¶¶¶
The higher prevalence of rectal signs and symptoms among persons with HIV infection could be related to differences in site of exposure, increased biologic susceptibility, or other factors. Rectal signs and symptoms did not vary by HIV immune status (CD4 count <350/μL versus ≥350 μL), supporting differences in site of exposure as a likely explanation. In a prospective cohort in Spain, MSM with monkeypox who engaged in receptive anal sex were more likely to report proctitis and systemic signs and symptoms preceding rash (3). When evaluating patients with rectal signs and symptoms, care providers should consider monkeypox and the possibility of concurrent rectal STIs. Understanding whether rectal signs and symptoms can precede rash onset or occur when rash is absent or unrecognized (because of anatomic site or small number of lesions) will help inform guidance for Monkeypox virus testing and new diagnostic approaches.
Limited data suggest that persons with HIV infection, particularly those with low CD4 counts or without HIV viral suppression, were more commonly hospitalized during their monkeypox illness than were persons without HIV infection. However, because data on reason for hospitalization are incomplete, it is not known whether this represents more severe monkeypox illness. Ongoing monitoring of outcomes of monkeypox by HIV infection status is important (7).
The findings in this report are subject to at least five limitations. First, this analysis was limited to diagnosed and reported monkeypox cases in eight jurisdictions and might not be generalizable to all U.S. monkeypox cases. Second, incomplete data on clinical signs and symptoms and hospitalization might affect the associations observed by HIV infection status. Third, some persons with undiagnosed HIV infection might have been misclassified as not having HIV, which could reduce differences in outcomes by HIV infection status. Fourth, local matching might have underestimated the prevalences of HIV infection and STIs by not including diagnoses reported in other jurisdictions or recent diagnoses. Finally, this analysis did not assess the relative contribution of structural, social, behavioral, or biologic factors to higher HIV infection and STI prevalences among persons with monkeypox. Further studies could improve understanding of such factors, monkeypox outcomes, and the impact of vaccination and treatment.
Public health efforts should continue to ensure equitable access to monkeypox screening, prevention, and treatment, particularly among MSM. It is important that systems for delivering HIV and STI care and prevention be leveraged for monkeypox evaluation, vaccination and other prevention interventions, and treatment (10). Data on diagnosis of HIV infections and STIs in close temporal association to monkeypox diagnosis reinforce the importance of offering recommended testing, prevention, and treatment services for HIV, STIs, and other syndemic conditions to MSM and other persons evaluated for monkeypox.**** Routine matching of monkeypox, HIV, and STI surveillance data to monitor trends and clinical characteristics of persons with coinfections can further inform public health interventions.
Top
Monkeypox, HIV, and STI Team
Michael Abassian, California Department of Public Health; Meaghan Abrego, New York State Department of Health; David Addo, District of Columbia Department of Health; Bridget J. Anderson, New York State Department of Health; Connie Austin, Illinois Department of Public Health; Kailey Bradley, Georgia Department of Public Health; David Bui, California Department of Public Health; Shua Chai, California Department of Public Health; Eric Chapman, California Department of Public Health; Joseph Clement, San Francisco Department of Public Health; Catherine Comis, Georgia Department of Public Health; Phoebe Danza, Los Angeles County Department of Public Health; Marisa Donnelly, California Department of Public Health; Kerri Dorsey, District of Columbia Department of Health; Kate Drezner, District of Columbia Department of Health; Alicia Dunajcik, CDC Monkeypox Emergency Response Team; Areesh Fatmee, District of Columbia Department of Health; Amanda Feldpausch, Georgia Department of Public Health; Lauren Finn, Los Angeles County Department of Public Health; Rebecca Fisher, Los Angeles County Department of Public Health; Kameron Gadawski, Georgia Department of Public Health; Jasmine Gaillard, CDC Monkeypox Emergency Response Team; Varun Gandhi, New York State Department of Health; Amy Garlin, San Francisco Department of Public Health; Sarah Gillani, District of Columbia Department of Health; Jamilla Green, CDC Monkeypox Emergency Response Team; Megan Hill, Georgia Department of Public Health; Taylor Holly, Chicago Department of Public Health; Virginia Hu, Los Angeles County Department of Public Health; Otto Ike, CDC Monkeypox Emergency Response Team; Anna Satcher Johnson, CDC Division of HIV Prevention; Kelly Johnson, California Department of Public Health; Janna Kerins, Chicago Department of Public Health; David Kern, Chicago Department of Public Health; Bita Khoshhal, Georgia Department of Public Health; Akiko Kimura, California Department of Public Health; Irma Kocer, CDC Monkeypox Emergency Response Team; Colin Korban, Chicago Department of Public Health; Chun-Mai Kuo, Los Angeles County Department of Public Health; Rodriques Lambert, Georgia Department of Public Health; Issa Lee-Hall, CDC Monkeypox Emergency Response Team; Jessica Lorenzo-Luaces, Georgia Department of Public Health; Elise Mara, San Francisco Department of Public Health; Amy Marutani, Los Angeles County Department of Public Health; Karla Miletti, District of Columbia Department of Health; Wilson Miranda, New York State Department of Health; Allison Morrow, District of Columbia Department of Health; Dawn Nims, Illinois Department of Public Health; Melissa Ongpin, San Francisco Department of Public Health; Chisom Onyeuku, CDC Monkeypox Emergency Response Team; Jessica Pavlick, Georgia Department of Public Health; Eugene Pennisi, Georgia Department of Public Health; Neela Persad, CDC Monkeypox Emergency Response Team; Mary Pomeroy, CDC Monkeypox Emergency Response Team; Kathleen Poortinga, Los Angeles County Department of Public Health; Dylan Atchley Procter, Georgia Department of Public Health; Marisa Ramos, California Department of Public Health; Eli Rosenberg, New York State Department of Health; Lori Saathoff-Huber, Illinois Department of Public Health; Nannie Song, California Department of Public Health; Dan Stowell, CDC Monkeypox Emergency Response Team; Deanna Sykes, California Department of Public Health; Amanda Terminello, CDC Monkeypox Emergency Response Team; Ebony Thomas, CDC Monkeypox Emergency Response Team; Chris Toomey, San Francisco Department of Public Health; Brittany Wilbourn, District of Columbia Department of Health; Tanya Williams, CDC Monkeypox Emergency Response Team; Pascale Wortley, Georgia Department of Public Health.
https://www.cdc.gov/mmwr/volumes/71/wr/mm7136a1.htm?s_cid=mm7136a1_w
Créditos: Comité científico Covid




