En atención a la creciente preocupación sobre la confianza en...
Leer más
The COVID Heart—One Year After SARS-CoV-2 Infection, Patients Have an Array of Increased Cardiovascular Risks
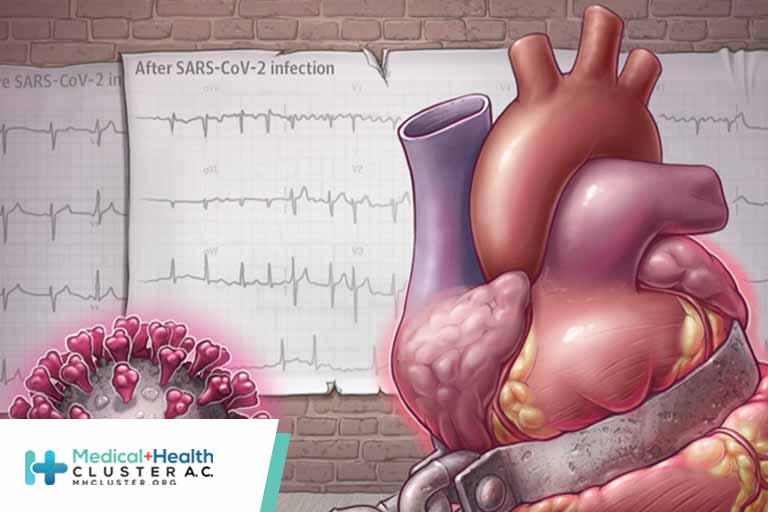
An analysis of data from nearly 154 000 US veterans with SARS-CoV-2 infection provides a grim preliminary answer to the question: What are COVID-19’s long-term cardiovascular outcomes? The study, published in Nature Medicine by researchers at the Veterans Affairs (VA) St Louis Health Care System, found that in the year after recovering from the illness’s acute phase, patients had increased risks of an array of cardiovascular problems, including abnormal heart rhythms, heart muscle inflammation, blood clots, strokes, myocardial infarction, and heart failure. What’s more, the heightened risks were evident even among those who weren’t hospitalized with acute COVID-19.
The Backstory
At the beginning of the pandemic, the research team resolved to identify and address important knowledge gaps around COVID-19, study senior author Ziyad Al-Aly, MD, told JAMA in an email. “At that time, none of us knew anything about long COVID,” noted Al-Aly, who is chief of research and development at the VA St Louis Health Care System and a clinical epidemiologist at Washington University in St Louis. “Over several weeks, we started hearing about patients who were not fully recovering and had lingering issues including heart problems.” These patients—who call themselves long haulers—inspired the team to study long COVID, also known as post-COVID conditions.
In a report published in Nature last April, the researchers demonstrated that people with long COVID can have sequelae in several organ systems, including cardiovascular disorders. With the current study, they set out to gain a deeper understanding of COVID-19’s long-term cardiovascular consequences.
The Design
The new analysis in Nature Medicine examined a comprehensive, prespecified set of cardiovascular outcomes among patients in the US Veterans Health Administration (VHA) system who survived the first 30 days of COVID-19. The researchers estimated the risks and excess burden of cardiovascular outcomes per 1000 persons 12 months after COVID-19 using electronic medical record data from 3 large cohorts:
-
153 760 patients who used VHA services in 2019 and had a positive SARS-CoV-2 test result between March 1, 2020, and January 15, 2021
-
5 637 647 patients with no evidence of SARS-CoV-2 infection who used VHA services in 2019—the contemporary control group
-
5 859 411 prepandemic patients who used VHA services in 2017—the historical control group
The cohorts largely comprised older White male patients. The COVID-19 cohort, which averaged 61 years old, included 89% males and about 71% White individuals. But because the study was large, it also included almost 17 000 female patients; about 37 000 Black patients; and almost 8000 Latino, Asian, American Indian, Native Hawaiian, and patients of other races with COVID-19.
What We’ve Learned
Patients with COVID-19 were at increased risk of a broad range of cardiovascular disorders including cerebrovascular disorders, dysrhythmias, ischemic and non–ischemic heart disease, pericarditis, myocarditis, heart failure, and thromboembolic disease.
At the 12-month mark, compared with the contemporary control group, for every 1000 people, COVID-19 was associated with an extra:
-
45.29 incidents of any prespecified cardiovascular outcome
-
23.48 incidents of major adverse cardiovascular events (MACEs), including myocardial infarction, stroke, and all-cause mortality
-
19.86 incidents of dysrhythmias, including 10.74 incidents of atrial fibrillation
-
12.72 incidents of other cardiovascular disorders including 11.61 incidents of heart failure and 3.56 incidents of nonischemic cardiomyopathy
-
9.88 incidents of thromboembolic disorders, including 5.47 incidents of pulmonary embolism and 4.18 incidents of deep vein thrombosis
-
7.28 incidents of ischemic heart disease including 5.35 incidents of acute coronary disease, 2.91 incidents of myocardial infarction, and 2.5 incidents of angina
-
5.48 incidents of cerebrovascular disorders, including 4.03 incidents of stroke
-
1.23 incidents of inflammatory disease of the heart or pericardium, including 0.98 incidents of pericarditis and 0.31 incidents of myocarditis
Patients with more severe disease—determined by whether they recuperated at home, were hospitalized, or were admitted to the intensive care unit—had higher risks. But the risks were evident even among those who were not hospitalized with COVID-19. Other subgroup analysis found increased risks regardless of age, race, sex, obesity, smoking, hypertension, diabetes, chronic kidney disease, hyperlipidemia, and preexisting cardiovascular disease.
The study’s overall findings were consistent when outcomes were compared between patients with COVID-19 and the control group of prepandemic patients.
A Note on Myocarditis
Because some COVID-19 vaccines may be associated with rare cases of myocarditis and pericarditis, the authors conducted analyses to remove the effect of vaccination. The increased risk of myocarditis and pericarditis remained among people who were not vaccinated and was evident regardless of vaccination status.
The Surprises
The increased risks were most pronounced for heart failure and atrial fibrillation, but the breadth of cardiovascular disease involvement was “eye opening,” Al-Aly wrote in his email. The researchers also were surprised to see elevated risks for people who were not hospitalized for COVID-19 during the acute phase—the segment that represents the majority of people with SARS-CoV-2 infection. However, the study did not analyze symptomatic vs asymptomatic infections, a potential area for further research.
Al-Aly said the subgroup analyses also rendered surprising results. He went into the project thinking the health issues would be evident among people with high risk of cardiovascular disease, “but the data showed that COVID-19 may be an equal opportunity offender,” he wrote. “The risks were evident in young people and old people, in Black people and White people, in males and females, in people who smoke and people who do not smoke, in people who have diabetes, and people without diabetes, etc. It really did not spare any subgroup.”
It’s possible that for some individuals, cardiovascular risks—such as obesity and chronic kidney disease—and preclinical cardiovascular disease increased the risk of acquiring SARS-CoV-2 infection in the first place and led to worse cardiovascular outcomes after COVID-19, Al-Aly noted. However, the increased risk across the board in all study subgroups “likely suggests that infection with SARS-CoV-2 is also leading to de novo cardiovascular disease,” he wrote.
The Clinical Takeaway
Physicians should consider a history of COVID-19 as a cardiovascular disease risk. “We think it is important to pay close attention to people with COVID-19 and identify early signs or symptoms of heart disease,” Al-Aly wrote. He emphasized that early identification, diagnosis, and treatment will be key to lessening the risk of further downstream adverse health consequences.
Recognizing the COVID Heart
The study demonstrates that cardiovascular disease is 1 facet of the multifaceted disorder known as long COVID, according to Al-Aly. He emphasized that long COVID is not only fatigue or brain fog but rather the constellation of symptoms and organ dysfunction that result from COVID-19 and persist or arise anew in the postacute phase of the disease.
As the pandemic enters its third year, Al-Aly said a coordinated global response strategy is urgently needed to address the challenges of dealing with the long-term health effects of COVID-19, an enterprise he called a “long COVID moonshot.”
“I think there are a lot of knowledge gaps that need to be investigated in future research to gain a better understanding of the health trajectories of people with a COVID heart (cardiovascular COVID) and their long-term outcomes,” he noted. How best to identify, diagnose, and treat these patients is a critical area of future research.
The Last Word
“In our work, we show serious long-term cardiovascular disease consequences of COVID-19,” Al-Aly wrote. “Most of these are lifelong conditions that will affect people for a lifetime and may impact their quality of life and other health outcomes. The risks reported in our paper may appear small but given the large number of people with COVID-19 in the US and globally, these numbers will likely translate into millions of people with heart disease in the US and many more around the world. We need to realize this now and make sure we are prepared and ready to address the needs of these patients.”
Créditos: Comité científico Covid




