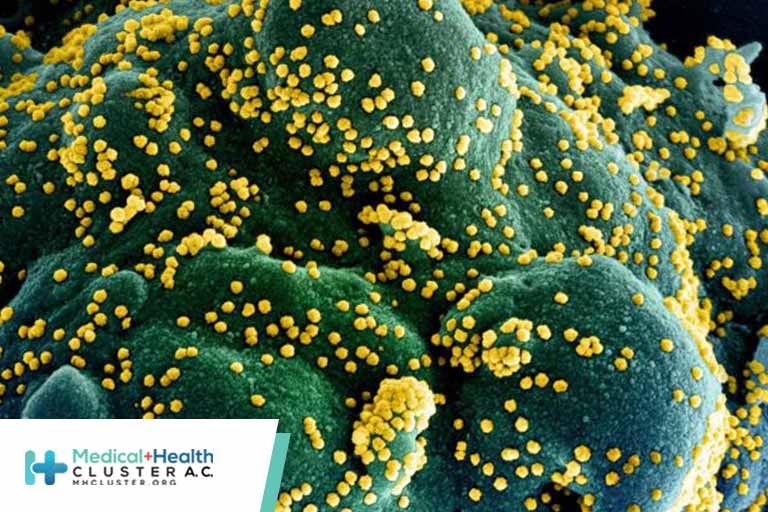
Researchers at Arizona State University and the University of Washington have reported a novel method for detecting viruses such as SARS-CoV-2 and Ebola.
The usual methods of detecting these viruses are ELISA (enzyme-linked immunosorbent assay) or PCR (polymerase chain reaction). ELISA is like a lock and key and is most commonly used to measure an antibody that locks to an antigen affixed to a specially coated 96-well plastic plate with a colorimetric test. The more antibodies present, the more intense the color.
In PCR, a specific DNA sequence is amplified with a primer: a short, single strand of DNA. Dyes attached to the primer measure the amount of DNA present, in this case the amount of the viral antigen. It requires several pieces of specialized equipment, chemicals, and training. ELISAs are easier. They have good sensitivity but less specificity than PCRs.
But both ELISA and PCR have shortcomings, especially the need for specialized equipment and training. ELISA requires someone to handle the reactions on the plate and a spectrophotometer to measure the optical density of the reaction, which is translated by a computer into the amount of antibody present. PCRs also require thermal cyclers and a reader to measure the amount of dye linked to the sample.
The answer, say the researchers, may lie in “nanobodies” and the “nanosensors” that can detect them.
They have named their assay “Nano2RED,” after the nanosensors it uses and its rapid electronic detection.
Nanobodies are tiny, single-domain antibody fragments. They were initially isolated from camelids (camels, llamas, and alpacas). But now they can be synthesized.
Through a high throughput screening method called phage display, nanobodies that bind to a specific antigen can quickly be identified. Streptavidin, a stable protein with a very high affinity to biotin, is that antigen and makes a very stable compound. This biotin-streptavidin interaction helps the nanobodies to stick to gold nanoparticles. The gold compound acts as a probe, identifying the antigen. When exposed to the antigen, the gold particles will clump, and these heavier, bound clusters of gold nanoparticles and antigens sink to the bottom of the test tube.

Dr Chao Wang
Chao Wang, PhD, from Arizona State University in Tempe, described the process to Medscape Medical News. In their assay, results are displayed as a color change, measured via LEDs and photodetectors. But in contrast to traditional ELISA assays, the more antigen, the lighter the color.
Wang’s lab invented a device that converts the color absorbed by the gold particles to an electrical signal as light is passed through a test tube. Then, they obtain quantitative colorimetric, spectrometric, and electronic readouts that show the amount of antigen present (and thus a measure of infection).
In describing the assay, Wang said their technology has the advantages of being inexpensive (about 1 cent per test) and rapid (15-20 minutes). It can use a portable digital readout system, essential for quantifying the amount of antigen present. It is also 10 times more sensitive than ELISA-type assays.
Wang also said that this technology could readily be adapted to other antigens or future infections. Their research was supported by the National Science Foundation and the National Institutes of Health.

Dr Robert Meagher
Robert Meagher, PhD, a technical staff member at Sandia National Laboratories, told Medscape Medical News that this approach incorporates elements that are regularly used elsewhere, such as phage display technology. “Gold nanoparticles conjugated to antibodies are actually a pretty common reagent used for signal amplification in rapid antigen tests — gold nanoparticles are what generate the pink signal line on a standard rapid antigen test,” Meagher said.
Similarly, other groups are using nanobodies. For example, Meagher said, his Sandia colleague Brooke Harmon “published a paper recently, where her team did exactly that part of this process to find the antibodies that will bind to neutralize SARS-CoV-2. That was published and they now have antibodies that will see and recognize all the different variants of COVID.”
But Meagher also expressed several concerns. For one, while using small blood samples for Ebola makes sense, “SARS-CoV-2 is not bloodborne, so respiratory samples like nasal swabs are the normal sample there. I’m not sure why they used blood or serum as a model sample for SARS-CoV-2 spike protein.”
A more serious concern is the “signal-off” mechanism. “It’s always better if it’s no color, and then you add the antigen, and you develop color,” Meagher said. “I think it’s more subjective to interpret.”
Another newly reported diagnostic test is a SmaRT-LAMP (loop-mediated isothermal amplification) assay, described in the journal JAMA Network Open. The project lead is Michael Mahan, PhD, professor of molecular, cellular, and developmental Biology at the University of California, Santa Barbara, working with other scientists at UCSB and Cottage Hospital.
Meagher also commented on this paper. He noted this is not directly comparable to Wang’s assay because it is molecularly based rather than measuring antigen. In addition to being more sensitive, it is also (relatively) inexpensive and requires little more than saliva, a hot plate, a smartphone, a chemical assay, and a 96-well plate. It meets the World Health Organization’s “ASSURED” criteria: affordable, sensitive, specific, user-friendly, rapid/robust, equipment-free, and deliverable. It also meets those for REASSURED: real-time connectivity and ease of specimen collection and environmental friendliness.
Mahan’s group is not patenting their technology, and everything is open access.
Meagher concluded that Wang’s group had “done the basic development showing some proof of concept with model samples. This particular work probably has some further development before it could be as easy to use as the current rapid antigen tests. It’s hard to tell whether it has advantages in sensitivity, but in its present form, it looks like it’s not quite as easy as a lateral flow antigen test.”
Wang has filed two patent applications. Meagher has disclosed no relevant financial relationships.
Biosensors and Bioelectronics. Published online January 6, 2022. Full text.