En atención a la creciente preocupación sobre la confianza en...
Leer más
Long Covid and Impaired Cognition — More Evidence and More Work to Do

During the early stages of the Covid-19 pandemic, reports emerged that persons who had been infected with SARS-CoV-2 were having lingering health problems. Such long-term issues were collectively referred to as “long Covid” and were reported to affect nearly every organ system.1 The cardinal features of long Covid include fatigue, dysautonomia (or postural orthostatic tachycardia syndrome), postexertional malaise, and cognitive difficulties that are colloquially referred to as “brain fog.”
Several large studies then emerged documenting the presence of neurologic sequelae — including cognition and memory problems — in the postacute phase of SARS-CoV-2 infection.2,3 A recent analysis of the U.S. Current Population Survey showed that after the start of the Covid-19 pandemic, an additional one million U.S. residents of working age reported having “‘serious difficulty’ remembering, concentrating, or making decisions” than at any time in the preceding 15 years.4 Whether these changes are attributable solely to long Covid is unclear, but that report represents a change in the cognitive health of U.S. residents from prepandemic levels.
In a study published in this issue of the Journal, Hampshire et al.5 bring greater clarity to how SARS-CoV-2 infection may affect cognition. They studied 800,000 adults from a larger community sample of more than 3 million persons in the Real-Time Assessment of Community Transmission (REACT) study of SARS-CoV-2 transmission in England. Using an online assessment tool for cognitive function with eight domains, the investigators estimated global cognitive scores among participants who had been previously infected with SARS-CoV-2 and had had symptoms that persisted at least 12 weeks, whether resolved or not, and among uninfected participants.
Modest cognitive decline occurred with the original virus and with each viral variant, including B.1.1.529 (omicron). As compared with uninfected participants (control), cognitive deficit — commensurate with a 3-point loss in IQ — was evident even in participants who had had mild Covid-19 with resolved symptoms. Participants with unresolved persistent symptoms had the equivalent of a 6-point loss in IQ, and those who had been admitted to the intensive care unit had the equivalent of a 9-point loss in IQ. Of importance, these deficits were associated with many of the other symptoms that have been reported by persons with long Covid. The greatest deficits in cognitive function were associated with the original strain of the virus (before December 1, 2020) and the early B.1.1.7 (alpha) variant (from December 1, 2020, to April 30, 2021). Longer hospital stays and durations of acute illness were predictors of persistent global deficits. Memory, reasoning, and executive function (i.e., planning) tasks were the most sensitive indicators of impaired function, and scores on these tasks tended to correlate with brain fog. Vaccinations provided a small cognitive advantage. Reinfection contributed an additional loss in IQ of nearly 2 points, as compared with no reinfection.
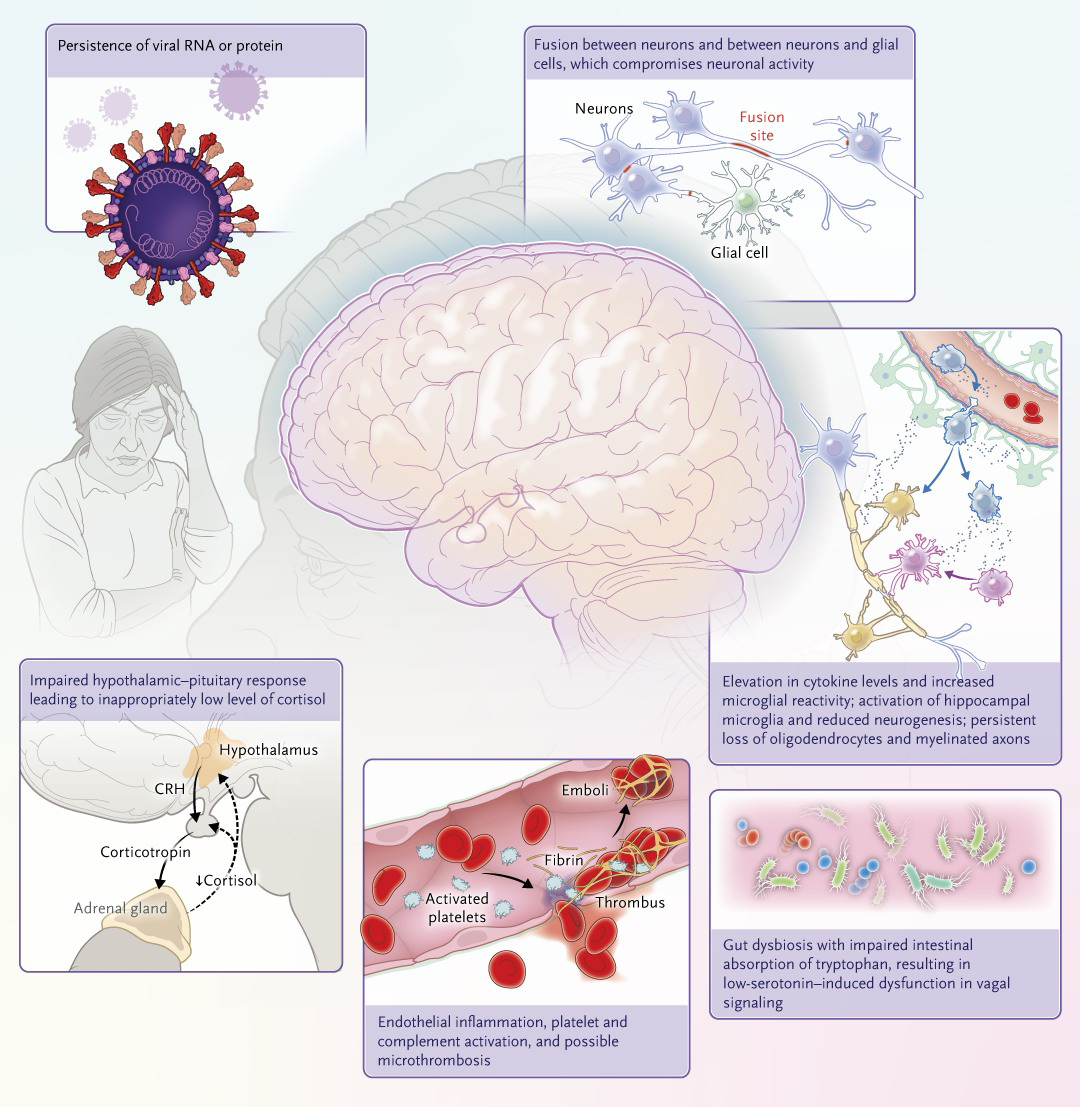
The mechanisms of cognitive dysfunction after SARS-CoV-2 infection still need to be elucidated (Figure 1). Studies involving humans and mouse organoids showed that SARS-CoV-2 infection induces fusion of neurons, which compromises neuronal activity. Studies involving humans have shown prolonged neuroinflammatory responses, structural abnormalities, and accelerated aging in the brains of persons with mild-to-moderate SARS-CoV-2 infection.6-8 Virus was present in brain-tissue samples obtained during autopsy from persons who had had severe Covid-19.8 Gut dysbiosis, dysfunctional hypothalamic–pituitary response, and low-serotonin–induced dysfunction in vagal signaling may also play a role in impaired cognition after SARS-CoV-2 infection.9,10
The results of the study by Hampshire and colleagues are of concern, and the broader implications require evaluation. For example, what are the functional implications of a 3-point loss in IQ? Whether one group of persons is affected more severely than others is not clear. Whether these cognitive deficits persist or resolve along with predictors and trajectory of recovery should be investigated. Will Covid-19–associated cognitive deficits confer a predisposition to a higher risk of Alzheimer’s disease or other forms of dementia later in life? The effects on educational attainment, work performance, accidental injury, and other activities that require intact cognitive abilities should also be evaluated. SARS-CoV-2 infection happened in the context of a global pandemic that disrupted many facets of our lives; disentangling the effects of the infection from those of the pandemic (e.g., social isolation, grief, and trauma) should also be undertaken.
There are limitations to the study conducted by Hampshire and colleagues. The study was based on an engagement survey; hence, there may be a degree of response and ascertainment bias, such that either more persons with long Covid may have opted to enroll and that persons who were sick and had disability would not participate in the surveys. Also, there was a lack of racial diversity, which will lead to uncertainty with regard to the effects of long Covid on cognition in underrepresented populations.
The SARS-CoV-2 pandemic produced in its wake millions of persons affected with long Covid, some of whom have had or are currently having cognitive challenges. A deeper understanding of the biology of cognitive dysfunction after SARS-CoV-2 infection and how best to prevent and treat it are critical for addressing the needs of affected persons and preserving the cognitive health of populations.
Source: https://www.nejm.org/doi/full/10.1056/NEJMe2400189?fbclid=IwAR0gUgnoe1T_DYx3TYil9nPBPlp11U-Ofp-RHil27qIRV8UlUmj8m4cuOPI




