CONDENA MH CLÚSTER ATAQUE ARMADO A HOSPITAL ARCÁNGELES
Leer más
What to Know About EG.5, the Latest SARS-CoV-2 “Variant of Interest”
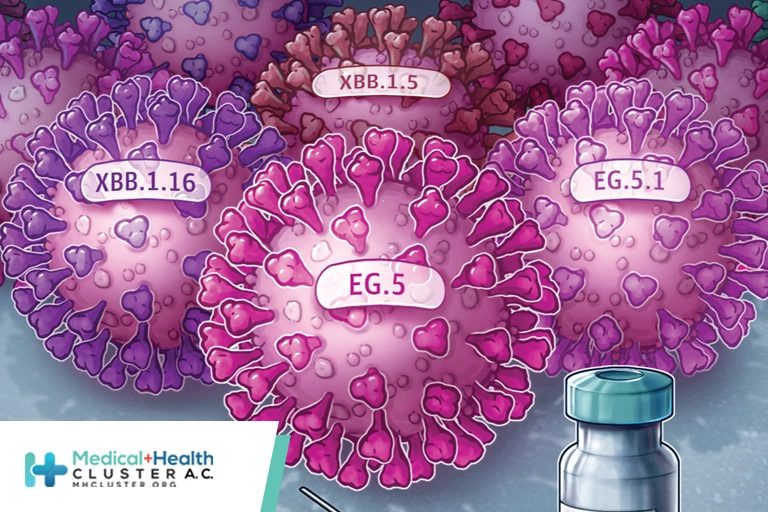
The Omicron descendant EG.5 is the latest to be labeled a “variant of interest” by the World Health Organization (WHO), joining the current ranks of XBB.1.16 and XBB.1.5. The new designation, made as part of an August 9 initial risk evaluation of the variant, reflects its “notable rise” in global prevalence during recent weeks.
The report comes as the US is experiencing an increase in hospitalizations and deaths and as anticipation mounts for updated vaccines, expected to become available this fall. The EG.5 variant could contribute to a surge in cases, the report noted, although there’s no evidence to date that it causes more severe disease.
For now, the report concludes, the new variant doesn’t seem to pose a greater public health risk than others that are circulating. That said, it cautions that currently, variant surveillance isn’t representative and variant reporting isn’t reliable. These factors are creating data gaps—a barrier to comprehensively evaluating EG.5′s risks.
Here’s what’s currently known about the variant and how it could shape the COVID-19 situation in the coming months.
It Has a Growth Advantage
The WHO risk evaluation determined that EG.5 has a moderate growth advantage. The variant was first reported to the WHO in February, and its share of reported sequences has increased steadily since then. Its global prevalence more than doubled this summer, from about 8% the week ending June 25 to about 17% the week ending July 23.
It was not yet globally ascendant at press time, based on the most recent data available. An August 10 epidemiological update from the WHO noted that XBB.1.16 was the most prevalent variant around the world during the week ending July 23, representing a quarter of virus sequences. XBB.1.5 was on the decline, accounting for about 13% of sequences.
But EG.5.1, a subvariant that represents most EG.5 sequences, has a higher effective reproduction number than those XBB variants, according to a study posted to the preprint server bioRxiv, which has not yet been peer-reviewed. This finding suggests that EG.5 and its sublineages could predominant “in the near future,” virologist Kei Sato, PhD, senior author of the study and a professor at the Institute of Medical Science at the University of Tokyo in Japan, wrote in an email to JAMA.
EG.5 is already the fastest growing variant in several areas of the world. In the US, it and its sublineages likely overtook both XBB.1.16 and XBB.1.5 by early August, per projections from the Centers for Disease Control and Prevention (CDC).
It Has Antibody Escape Properties
EG.5 is descended from XBB.1.9.2, an Omicron offspring with the same spike protein as XBB.1.5, the variant targeted by the forthcoming vaccines. But unlike those variants, EG.5 has the spike protein mutation F456L, which in laboratory experiments allowed it to evade most XBB.1.5-neutralizing antibodies. The EG.5.1 subvariant, which accounts for 88% of available EG.5 sequences, contains an additional spike protein mutation, Q52H.
The F456L mutation appears to be especially important, Sato and others said.
“F456L in particular has come up repeatedly in descendants of XBB.1.5 and may make it slightly less susceptible to antibodies in previously vaccinated and/or infected people,” Nicole Doria-Rose, PhD, a National Institutes of Health (NIH) staff scientist, said in an email. F456L may also be linked to transmissibility, noted Doria-Rose, who is chief of the Humoral Immunology Core at the National Institute of Allergy and Infectious Diseases’ Vaccine Research Center.
Based on the current data, the WHO has classified EG.5′s antibody escape risk as moderate. The report cautioned, however, that the immune escape results are based on studies from a single laboratory using pseudotyped, not wild-type, viruses, and that additional experiments are needed to further assess how well EG.5 thwarts existing antibodies.
It’s Unclear Whether It’s Driving the COVID Wave
In the US, COVID-19 test positivity, wastewater levels, emergency department visits, hospitalizations, and deaths are all rising, based on CDC data through the first week of August. However, it’s unclear to what extent EG.5 could be driving the current wave. Sato said waning immunity from vaccinations and previous infections could be contributing.
It’s also important to note that hospitalizations and deaths in the US are still drastically lower than this time last year. Carlos del Rio, MD, a distinguished professor of medicine in the Division of Infectious Diseases at Emory University School of Medicine and president of the Infectious Diseases Society of America, said he’s “somewhat concerned” about current increase in hospitalizations, which he attributes mostly to XBB variants. “However,” he wrote in an email, “I also know if people are boosted, it is very unlikely they will end up hospitalized when infected.”
There’s No Indication It’s More Severe
So far there are no reports that EG.5 causes more severe COVID-19 cases, leading the WHO to classify its level of risk for severe disease as low.
“Several countries with rising EG.5 prevalence have seen increases in cases and hospitalizations, although at present there is no evidence of an increase in disease severity directly associated with EG.5,” the report noted.
Doria-Rose explained that EG.5 might be linked to the current increase in COVID-19 cases, and therefore hospitalizations, “based on its transmissibility, not its severity.”
There are caveats to the WHO risk assessment, though. Global reporting of new hospitalizations and intensive care unit admissions has fallen off substantially, so the WHO said it’s best to be cautious when interpreting the data on severe cases. And it said that more studies are needed to investigate the variant’s effect on clinical outcomes.
There’s Optimism About the Updated Vaccine Booster
The updated COVID-19 vaccines are expected to be available in the US in mid to late September, assuming they receive authorization from the US Food and Drug administration (FDA) and are recommended by the CDC, an FDA spokesperson told JAMA in an email. The big question is, will they be effective against EG.5?
Both del Rio and Doria-Rose said they think the monovalent XBB.1.5 boosters will offer some protection against EG.5, which is after all an XBB offshoot. (It’s also known as XBB.1.9.2.5.)
“Since there are very few changes from the XBB.1.5 spike protein, which is the basis of the vaccines for fall 2023, I would expect the new vaccines to work well against it, and better than last year’s vaccines which were based on ancestral and BA.5 strains,” Doria-Rose said.
David C. Montefiori, PhD, who directs the Laboratory for HIV and COVID-19 Vaccine Research & Development at Duke University Medical Center, echoed this in an email. “The fall vaccines are expected to continue to be highly effective against EG.5,” he said, adding that the F456L mutation “is not thought to have a major impact on the ability of the variant to escape the vaccine.”
Confirmation could come soon. Montefiori said his team and other researchers are currently testing serum samples from people who were boosted with the updated vaccine.
As of this May, only 17% of people in the US had received the original bivalent booster. For those who skipped a booster dose, del Rio said that at this point he recommends waiting the month or so until the updated vaccines become available. His message: “COVID ain’t over. Get your boosters as soon as possible.”
Source: https://jamanetwork.com/journals/jama/fullarticle/2808762?fbclid=IwAR1QiC8Slp2ahe1M2ZK904ow-nfqkCJ-JDF4JqycHZL2WnFLLXJd4ZtY2BA#:~:text=The%20EG.5%20variant%20could,than%20others%20that%20are%20circulating




