En atención a la creciente preocupación sobre la confianza en...
Leer más
Pediatricians and parents on the brink: This is their March 2020
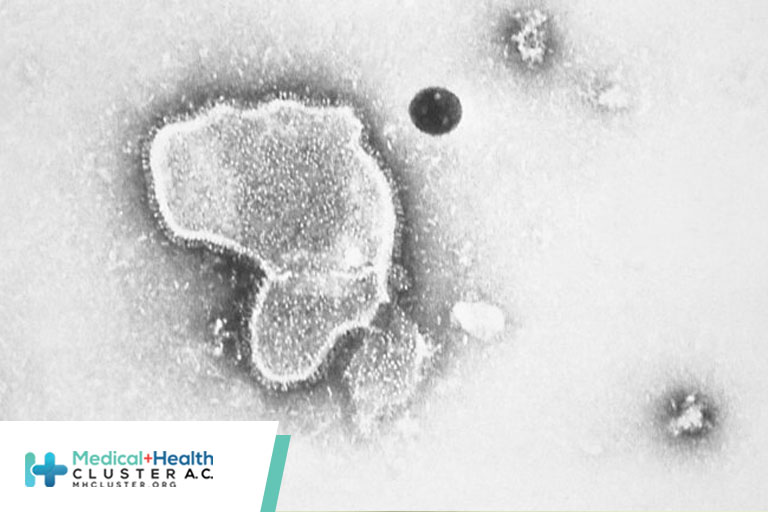
In March 2020, as the Covid-19 pandemic swept across the United States, the nation’s pediatric providers and pediatric units immediately pitched in to treat adults sickened by this then-mysterious and deadly disease. But now that the pediatric community is facing its own March 2020 with the confluence of Covid-19, influenza, and respiratory syncytial virus (RSV), the response from outside this community has been slow.
That says volumes about how the U.S. prioritizes — or more accurately doesn’t prioritize — the health of children.
In the spring of 2020, pediatric units were eerily quiet. Pediatric providers were reassigned to address the influx of adults stricken with Covid-19. The precautions put in place to “flatten the curve” of transmission of SARS-CoV-2, the virus that causes Covid-19, also changed the predictable course of seasonal respiratory viruses that typically fill pediatricians’ offices and hospitals’ pediatric units during the winter months. Only a minimal number of flu and RSV cases were seen, and other viruses appeared only at unexpected times of the year.
For two respiratory virus seasons, children remained healthier than ever, with common conditions such as asthma, bronchiolitis, and associated bacterial infections occurring at exceptionally low rates.
This lull should have raised antennas and been a time of preparation for when precautions were removed and the common respiratory viruses that severely affect children circulated again. That wearing masks, social distancing, and widespread testing for viral infections could significantly reduce the transmission of respiratory viruses, and thus the number of children becoming ill with them, should have been lessons learned and implemented for keeping children well. Instead, the U.S. has chosen to look the other direction. Health systems were lulled into maintaining reduced workforces and bed capacity modeled on pediatric volumes during the prior year.
As precautions are left behind, an overwhelming burden of viral respiratory diseases is taxing pediatric providers and adding considerable stress to families with infants and young children. Given the disproportionate impact of the Covid-19 pandemic on families, the nation’s children are in crisis, and the impact of this surge may be felt for decades. The large number of cases of severe bronchiolitis occurring in infants and toddlers may set up an epidemic of asthma in children will that continue for years to come.
Clearly, the U.S. sacrificed the health and education of children to support a crisis that disproportionately affected adults.
The surge in children with respiratory infections has created major staffing challenges for children’s hospitals and is a significant hardship for the pediatric workforce, one that is already beleaguered by a paucity of medical trainees selecting pediatrics as a specialty, a nursing shortage, and an ongoing mental health crisis in children. This has had ripple effects for already stressed parents who are trying to navigate the pandemic in the new world without masking or social distancing.
At the root of this dilemma is that, as a country, the U.S. underfunds health care for children in spite of convincing evidence that addressing the childhood precedents of adult disease is the best way to improve the health of the adult population.
The slim capacity and staffing for pediatric units and children’s hospitals is directly related to how poorly Medicaid and the Children’s Health Insurance Program, which insure more than half of U.S. children, reimburse physicians and pediatric facilities for the care they provide children, especially when compared to what Medicare pays for adult care. This discrepancy also leads to the long-standing disparity in pay for pediatricians compared to those of physicians who treat adults, further contributing to the shortages in the pediatric workforce. Health care is funded in a way that indicates that the health of children is less important than the health of adults, a short-sighted and expensive choice.
While the calamity of the current surge in respiratory infections in young children is similar to that faced by adults in March 2020, a national response has yet to materialize despite requests for declaration of a public health emergency from national pediatric organizations. Further, adding to the challenges on pediatric providers are the many medication shortages complicating treatment of pediatric respiratory infections.
To be sure, there have been exciting advances in vaccines and other ways to prevent RSV infections in infants in the last months, yet the pressure on regulators to approve these products or for government incentives to hasten vaccine development — as there were with Covid-19 vaccines and treatments — have not been offered. Solutions for the national nursing or medication shortages or resources for health systems that serve Medicaid-funded pediatric populations have not been proposed.
The pediatric community is asking for the same response that health care systems gave to adults in the early pandemic, including incentives for relevant vaccine development, funding for the shrinking workforce and pediatric-focused health systems, and aid to families who have lost hope that the nation sees their plight.
Perhaps this pediatric respiratory illness crisis, layered on top of a youth mental health crisis, can jolt the country into action to address the inappropriately low Medicaid reimbursement rates that fund health care for the majority of the nation’s children. The country must respond quickly and passionately. Prioritizing children’s health is key to the nation’s health.
Sallie Permar is pediatrician-in-chief at NewYork-Presbyterian Komansky Children’s Hospital and chair of the Department of Pediatrics at Weill Cornell Medicine. She reports having consulted for Merck, Moderna, Dynavax, Hoopika, and Pfizer in regard to their cytomegalovirus vaccine programs. Robert Vinci is a pediatrician, chief of pediatrics at Boston Medical Center, chair of the Department of Pediatrics at Boston University School of Medicine, and a volunteer for the National Board for the Association of Medical School Pediatric Department Chairs.
Fuente:www.statnews.com/2022/12/06/covid-influenza-rsv-pediatricians-parents/?utm_campaign=facebook_organic&utm_medium=social&utm_source=facebook&fbclid=IwAR0dl_Q7LX3ni0oMtP6uLqrCvS7HO7vJw9LvO1dA5oTh2fSWLt9lwhllUL4




