CONDENA MH CLÚSTER ATAQUE ARMADO A HOSPITAL ARCÁNGELES
Leer más
Effectiveness of 2-Dose Vaccination with mRNA COVID-19 Vaccines Against COVID-19–Associated Hospitalizations Among Immunocompromised Adults — Nine States, January–September 2021
Summary
What is already known about this topic?
Studies suggest that immunocompromised persons who receive COVID-19 vaccination might not develop high neutralizing antibody titers or be as protected against severe COVID-19 outcomes as are immunocompetent persons.
What is added by this report?
Effectiveness of mRNA vaccination against laboratory-confirmed COVID-19–associated hospitalization was lower (77%) among immunocompromised adults than among immunocompetent adults (90%). Vaccine effectiveness varied considerably among immunocompromised patient subgroups.
What are the implications for public health practice?
Immunocompromised persons benefit from COVID-19 mRNA vaccination but are less protected from severe COVID-19 outcomes than are immunocompetent persons. Immunocompromised persons receiving mRNA COVID-19 vaccines should receive 3 doses and a booster, consistent with CDC recommendations, practice nonpharmaceutical interventions, and, if infected, be monitored closely and considered early for proven therapies that can prevent severe outcomes.
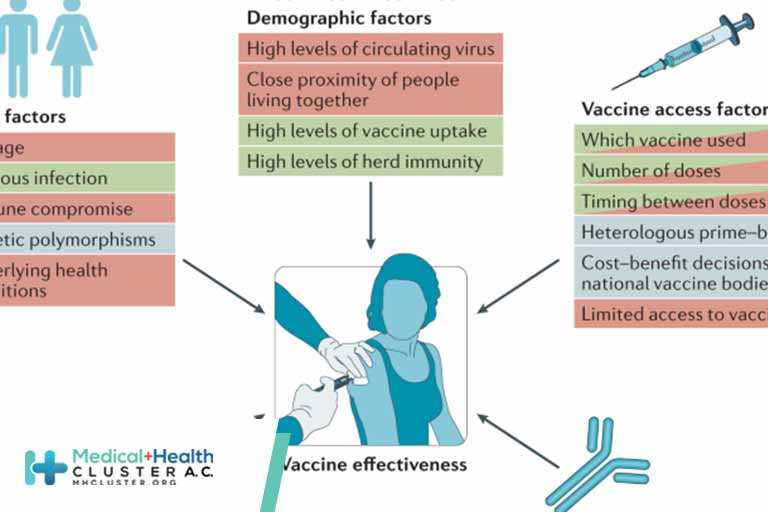
Immunocompromised persons, defined as those with suppressed humoral or cellular immunity resulting from health conditions or medications, account for approximately 3% of the U.S. adult population (1). Immunocompromised adults are at increased risk for severe COVID-19 outcomes (2) and might not acquire the same level of protection from COVID-19 mRNA vaccines as do immunocompetent adults (3,4). To evaluate vaccine effectiveness (VE) among immunocompromised adults, data from the VISION Network* on hospitalizations among persons aged ≥18 years with COVID-19–like illness from 187 hospitals in nine states during January 17–September 5, 2021 were analyzed. Using selected discharge diagnoses,† VE against COVID-19–associated hospitalization conferred by completing a 2-dose series of an mRNA COVID-19 vaccine ≥14 days before the index hospitalization date§ (i.e., being fully vaccinated) was evaluated using a test-negative design comparing 20,101 immunocompromised adults (10,564 [53%] of whom were fully vaccinated) and 69,116 immunocompetent adults (29,456 [43%] of whom were fully vaccinated). VE of 2 doses of mRNA COVID-19 vaccine against COVID-19–associated hospitalization was lower among immunocompromised patients (77%; 95% confidence interval [CI] = 74%–80%) than among immunocompetent patients (90%; 95% CI = 89%–91%). This difference persisted irrespective of mRNA vaccine product, age group, and timing of hospitalization relative to SARS-CoV-2 (the virus that causes COVID-19) B.1.617.2 (Delta) variant predominance in the state of hospitalization. VE varied across immunocompromising condition subgroups, ranging from 59% (organ or stem cell transplant recipients) to 81% (persons with a rheumatologic or inflammatory disorder). Immunocompromised persons benefit from mRNA COVID-19 vaccination but are less protected from severe COVID-19 outcomes than are immunocompetent persons, and VE varies among immunocompromised subgroups. Immunocompromised persons receiving mRNA COVID-19 vaccines should receive 3 doses and a booster, consistent with CDC recommendations (5), practice nonpharmaceutical interventions, and, if infected, be monitored closely and considered early for proven therapies that can prevent severe outcomes.
Data came from the VISION Network, a collaboration between CDC and seven U.S. health care systems and research centers with integrated medical, laboratory, and vaccination records that was established to assess the effectiveness of COVID-19 vaccines (6). Eligible hospitalizations were defined as those among adults aged ≥18 years with SARS-CoV-2 molecular testing (from 14 days before through 72 hours after admission) and a COVID-19–like illness discharge diagnosis.¶ Encounters without molecular testing were excluded from this analysis. Immunocompromised patients were defined by the presence of at least one selected discharge diagnosis for immunocompromising conditions using the International Classification of Diseases, Ninth Revision and International Classification of Diseases, Tenth Revision. Diagnoses across five categories of immunocompromising conditions were derived from lists used in previous studies of large hospital-based or administrative databases and included the following conditions: 1) solid malignancies, 2) hematologic malignancies, 3) rheumatologic or inflammatory disorders, 4) other intrinsic immune conditions or immunodeficiencies, and 5) organ or stem cell transplants (7–9). Immunosuppressive medication use data were not available for these analyses. Vaccination status was documented in electronic health records or state immunization registries (6). Full vaccination was defined as receipt of the second in a 2-dose series of Moderna (mRNA-1273) or Pfizer-BioNTech (BNT162b2) vaccines ≥14 days before the index hospitalization date; unvaccinated patients had not received any COVID-19 vaccine doses and were considered the referent group. Patients who received 1) only 1 mRNA vaccine dose, 2) ≥3 mRNA vaccine doses, 3) the second dose <14 days before index hospitalization date, or 4) the Janssen (Johnson & Johnson [Ad26.COV2]) vaccine were excluded from the analysis.
VE was estimated using a test-negative design comparing the odds of a positive test result for SARS-CoV-2 between fully vaccinated and unvaccinated patients using multivariable logistic regression models. VE was adjusted for age, geographic region, calendar time (days from January 1 to hospitalization), and local virus circulation in the community where each partner site was located and weighted for inverse propensity to be vaccinated or unvaccinated (calculated separately for each VE estimate). Generalized boosted regression trees were used to estimate the propensity to be vaccinated based on sociodemographic characteristics, underlying medical conditions, known previous SARS-CoV-2 infection, and hospital characteristics. VE estimates were stratified by immunocompromised status, mRNA COVID-19 vaccine product received, age group, and network partner (representing different health care systems and geographic regions). Among immunocompromised patients, VE was also calculated separately among subgroups of patients with each of the five categories of immunocompromising diagnoses (subgroups that were not mutually exclusive). VE was also calculated separately for hospitalizations occurring before and after the period when the Delta variant accounted for ≥50% of sequenced isolates within each site’s state (10). VE estimates with 95% CIs that did not overlap were considered statistically different, which is a conservative approach. This study was reviewed and approved by Westat, Inc. institutional review board.**
Among 69,116 immunocompetent adults and 20,101 immunocompromised adults hospitalized with COVID-19–like illness and with available molecular testing results for SARS-CoV-2, 29,456 (43%) and 10,564 (53%), respectively, were fully vaccinated (Table 1). The median ages of immunocompetent and immunocompromised patients were 68 years (interquartile range [IQR] = 52–79 years) and 70 years (IQR = 60–78 years), respectively. Among immunocompetent patients, 42% had received the Moderna vaccine and 58% had received the Pfizer-BioNTech vaccine, and among immunocompromised patients, 41% and 59% had received Moderna and Pfizer-BioNTech vaccines, respectively. Among immunocompetent patients, the median interval from receipt of the second vaccine dose to hospital admission was 89 days (IQR = 52–129 days) among Moderna vaccine recipients and 90 days (IQR = 52–131 days) among Pfizer-BioNTech vaccine recipients; among immunocompromised patients, the intervals were 89 days (IQR = 52–128 days) and 89 days (IQR = 53–128 days) for Moderna vaccine and Pfizer-BioNTech vaccine recipients, respectively.
Among immunocompetent patients, SARS-CoV-2 infection was laboratory-confirmed in 9,853 (24.8%) unvaccinated and 1,108 (3.8%) fully vaccinated persons, compared with 1,127 (11.8%) unvaccinated and 410 (3.9%) fully vaccinated immunocompromised patients (Table 2). VE of 2 doses of mRNA vaccine against COVID-19 hospitalization was lower among immunocompromised patients (77%) than among immunocompetent patients (90%). Differences persisted when analyzed among patients aged 18–64 years and aged ≥65 years, and among Moderna and Pfizer-BioNTech vaccine recipients. Among immunocompromised patients, VE was 81% for the Moderna vaccine and 71% for the Pfizer-BioNTech vaccine; however, CIs slightly overlapped between these two estimates. VE was similarly lower among immunocompromised than among immunocompetent patients both before the period of Delta variant predominance (76%; 95% CI = 69%–81% versus 91%; 95% CI = 90%–93%) and during the period of Delta variant predominance (79%; 95% CI = 74%–83% versus 90%; 95% CI = 89%–91%). Across network partners, VE point estimates varied more for immunocompromised patients (57–85%) than for immunocompetent patients (84%–94%).
Among immunocompromised patients, 8,887 (44%) had a solid malignancy, (range across network partners = 34%–47%), 2,790 (14%) a hematologic malignancy (range = 11%–19%), 5,024 (25%) a rheumatologic or inflammatory disorder (range = 22%–30%), 6,380 (32%) another intrinsic immune condition or immunodeficiency (range = 29%–37%), and 1,416 (7%) had received an organ or stem cell transplant (range = 4%–10%). VE point estimates ranged from 59% (organ or stem cell transplant patients) to 81% (patients with a rheumatologic or inflammatory disorder) across these subgroups (Table 3). Subgroup VE point estimates were generally higher for the Moderna vaccine than for the Pfizer-BioNTech vaccine but were the same among patients with a rheumatologic or inflammatory disorder.
Top
Discussion
In a multistate analysis of approximately 89,000 hospitalizations of adults with COVID-19–like illness during January 17–September 5, 2021, receipt of 2 doses of mRNA COVID-19 vaccine was effective in preventing laboratory-confirmed COVID-19 hospitalizations among patients who were immunocompromised (VE = 77%) and those who were immunocompetent (VE = 90%). Nonetheless, immunocompromised patients were significantly less protected from severe COVID-19 outcomes compared with immunocompetent patients, supporting the recommendation for administration of a third dose of mRNA vaccine to further enhance protection of moderately to severely immunocompromised persons against severe COVID-19 outcomes (5).
This study also found that VE was lower among certain subgroups of immunocompromised adults, such as solid organ or stem cell transplant recipients, than among others. These findings are consistent with other studies suggesting that certain immunocompromised persons experience an attenuated immune response to COVID-19 vaccines and make up a large proportion of hospitalizations for infections after vaccination (3,4). The prevalence of SARS-CoV-2 infection was approximately two times greater among unvaccinated immunocompetent patients compared with unvaccinated immunocompromised patients. Because the study sample was restricted to patients hospitalized with COVID-19–like illness, this difference might be related to a variation in the prevalence of other respiratory virus infections between the two groups, although this is unable to be confirmed. A strength of the test-negative design is that such a difference is not expected to influence the validity of VE estimates stratified by immunocompromised status.
The findings in this report are subject to at least six limitations. First, the use of selected discharge diagnoses as surrogates for presumed immunocompromised status and the absence of medication and other relevant data might have led to classification of persons as immunocompromised who were not; the opposite is also possible but is less likely. Second, selection bias might be possible if vaccination status influences the likelihood of receiving testing although a previous VISION Network study indicated that vaccination status did not affect receipt of testing (6). Third, despite the high specificity of COVID-19 vaccination status from these data sources, misclassification might be possible. Fourth, although inverse weights balanced unvaccinated and vaccinated hospitalized patients on sociodemographic and health characteristics, and further adjustments for age, geographic region, calendar time, and local virus circulation were made, unmeasured and residual confounding (e.g., mask-wearing and waning immunity) in this observational study might have biased these estimates. Fifth, the study only assessed mRNA COVID-19 vaccines and not the Janssen vaccine and included health care systems in only nine states, limiting the potential for the findings of this study to be extrapolated. Finally, immunocompromising conditions were not mutually exclusive, and sparse data in smaller immunocompromised subgroups reduced VE precision, so it was not possible to determine the independent effect of each subgroup on VE.
Immunocompromised persons benefit from and should receive COVID-19 vaccines. Given that VE is lower compared to immunocompetent patients, immunocompromised persons receiving mRNA vaccines should receive 3 doses and a booster 6 months after the third dose, consistent with CDC recommendations (5). In addition to vaccination, immunocompromised persons should implement nonpharmaceutical prevention strategies such as masking to help prevent SARS-CoV-2 infection, and, if infected with SARS-CoV-2, be monitored closely and considered early for proven therapies that might prevent progression to severe illness (e.g., monoclonal antibodies). Additional studies are needed to further characterize variation in VE among immunocompromised subpopulations and across geographic regions, determine the degree of improvements in VE conferred by additional COVID-19 vaccine doses in immunocompromised populations, evaluate whether different approaches to vaccine administration might improve VE (e.g., dosage timing or temporarily withholding immunosuppressants), and further evaluate possible differences in VE between vaccine products.
Créditos: Comité científico Covid




