En atención a la creciente preocupación sobre la confianza en...
Leer más
Nearly Half of Global Cancer Deaths Are Preventable
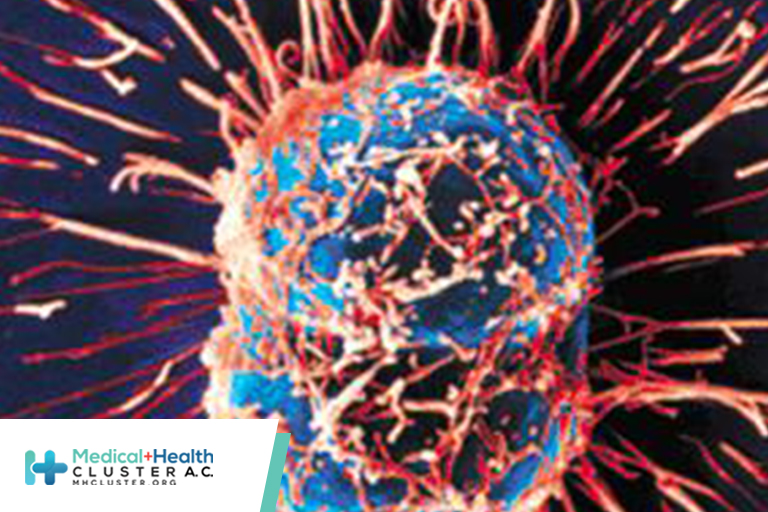
Nearly half of cancer deaths around the world are linked to preventable risk factors, which are largely behavioral, concludes a first-of-its-kind global report.
It found that the highest contributors are smoking, alcohol, and high body mass index (BMI), but it is the latter that is rather concerning. The highest increases in cancer deaths over the last decade relate to metabolic factors such as obesity, particularly in lower-income countries, the researchers point out.
“Smoking continues to be the leading risk factor for cancer globally,” the authors note. The leading cancers involved in risk-attributable deaths globally in 2019 for men and women were tracheal, bronchus, and lung cancer, representing 36.9% of all attributable cancer deaths.
The next most common risk-attributed cancers were colorectal, esophageal, and stomach cancer in men, and cervical, colorectal, and breast cancer in women.
“To our knowledge, this study represents the largest effort to date to determine the global burden of cancer attributable to risk factors,” say the authors.
“These findings highlight that a substantial proportion of cancer burden globally has potential for prevention through interventions aimed at reducing exposure to known cancer risk factors,” they add.
The study was published online in The Lancet.
“Our findings can help policymakers and researchers identify key risk factors that could be targeted in efforts to reduce deaths and ill health from cancer regionally, nationally, and globally,” co-author Christopher Murray, MD, director of the Institute for Health Metrics and Evaluation (IHME) at the University of Washington’s School of Medicine in Seattle, commented in a statement.
“The overriding message of this research is clear: a substantial proportion of cancers…is preventable,” write Diana Sarfati, MBChB, and Jason Gurney, PhD, of the University of Otago, New Zealand, in an accompanying editorial.
“Action to prevent cancer requires concerted effort within and outside the health sector,” they continue. “This action includes specific policies focused on reducing exposure to cancer-causing risk factors, such as tobacco and alcohol use, and access to vaccinations that prevent cancer-causing infections, including hepatitis B and HPV.”
“The primary prevention of cancer through eradication or mitigation of modifiable risk factors is our best hope of reducing the future burden of cancer,” they conclude.
Novel Project
The findings come from an analysis of the Global Burden of Diseases, Injuries, and Risk Factors (GBD) 2019 study, a novel project designed to quantify the cancer burden attributable to a wide array of modifiable risk factors in countries around the world, across factors including age, sex, and over time.
Outcomes including cancer deaths as well as disability-adjusted life-years (DALYs) were evaluated pertaining to 82 risk–outcome pairs, with 23 cancer types and 34 known risk factors, in the categories of behavioral, environmental and occupational, and metabolic risk factors, based on criteria from the World Cancer Research Fund.
The outcomes were evaluated for 2019, and changes in outcomes over time were assessed based on changes from 2010 to 2019.
Overall, the evaluated risk factors accounted for 44.4% of all cancer deaths, with the remaining cancers possibly not avoidable through control of the risk factors evaluated in the study.
Among men, the evaluated risk factors were involved in approximately half (50.6%) of all cancer deaths, whereas the rate was lower, about a third (36.3%), for women.
In 2019, the leading risk factors, globally, for both sexes were behavioral, and the top contributors were smoking, alcohol use, and high body mass index (BMI), although gender differences were observed.
Cancer DALYs attributable to smoking, for instance, were higher for men than women (33.2% vs 8.9%), as were DALYs attributed to alcohol (7.4% vs 2.3%).
Men were also more likely to have cancer deaths and DALYs attributable to environmental and occupational risks as well as behavioral risks compared with women.
Smoking, alcohol use, and high BMI were the largest contributors in higher-income regions according to their sociodemographic index.
However, in lower-income regions, the leading risk factors for risk-attributed cancer deaths were smoking, unsafe sex, and alcohol use.
Increases Over Time
Overall, the rates of cancer deaths associated with the evaluated risks increased by 20.4% between 2010 and 2019.
Of note, the increases over that time period were highest for cancer burden attributed to metabolic risks, which increased by 34.7% for cancer deaths.
The authors note that the increases in metabolic risks such as obesity were largely driven by increases in low- and low-middle–income countries, and could, in fact, be an unintended side effect of their progress.
“The growth in metabolic risk-attributable cancer burden might be the result of these countries experiencing an epidemiological transition in which improvements in country-level developmental status are related to increasing obesity levels,” they speculate.
Meanwhile, “globally, there has been substantial progress in reducing exposure to tobacco that can be linked to coordinated international and national prevention efforts.”
https://www.medscape.com/viewarticle/979461?src=soc_fb_220820_mscpedt_news_mdscp_cancer&faf=1#vp_1
Créditos: Comité científico Covid




