En atención a la creciente preocupación sobre la confianza en...
Leer más
COVID-19–Associated Hospitalizations Among U.S. Infants Aged Months — COVID-NET, 13 States, June 2021–August 2022
ummary
What is already known about this topic?
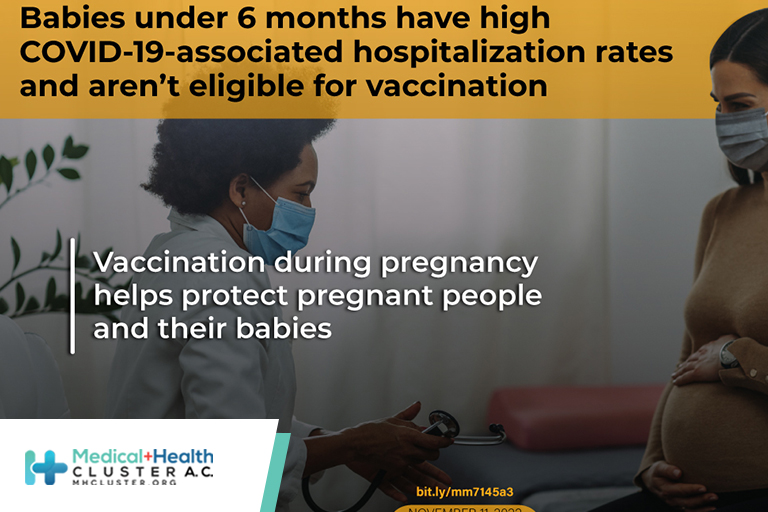
Infants aged <6 months, who are ineligible for vaccination, have high COVID-19–associated hospitalization rates compared with other pediatric age groups.
What is added by this report?
Although population-based COVID-19–associated hospitalization rates among infants aged <6 months increased in the Omicron variant–predominant periods compared with the Delta variant–predominant period, indicators of the most severe disease among hospitalized infants aged <6 months did not.
What are the implications for public health practice?
Pregnant women should stay up to date with COVID-19 vaccination to help protect themselves and infants too young to be vaccinated. Nonpharmaceutical measures should be used to help protect infants ineligible for vaccination.
COVID-19–associated hospitalization rates are highest among adults aged ≥65 years (1); however, COVID-19 can and does cause severe and fatal outcomes in children, including infants (2,3). After the emergence of the SARS-CoV-2 B.1.1.529 (Omicron) BA.1 variant in December 2021, hospitalizations among children aged <5 years, who were ineligible for vaccination, increased more rapidly than did those in other age groups (4). On June 18, 2022, CDC recommended COVID-19 vaccination for infants and children aged ≥6 months (5). Data from the Coronavirus Disease 2019–Associated Hospitalization Surveillance Network (COVID-NET)* were analyzed to describe changes in the age distribution of COVID-19–associated hospitalizations since the Delta-predominant period (June 20–December 18, 2021)† with a focus on U.S. infants aged <6 months. During the Omicron BA.2/BA.5–predominant periods (December 19, 2021–August 31, 2022), weekly hospitalizations per 100,000 infants aged <6 months increased from a nadir of 2.2 (week ending April 9, 2022) to a peak of 26.0 (week ending July 23, 2022), and the average weekly hospitalization rate among these infants (13.7) was similar to that among adults aged 65–74 years (13.8). However, the prevalence of indicators of severe disease§ among hospitalized infants did not increase since the B.1.617.2 (Delta)-predominant period. To help protect infants too young to be vaccinated, prevention should focus on nonpharmaceutical interventions and vaccination of pregnant women, which might provide protection through transplacental transfer of antibodies (6).
COVID-NET conducts population-based surveillance for laboratory-confirmed COVID-19–associated hospitalizations among residents of predefined surveillance catchment areas.¶ COVID-19–associated hospitalizations are defined as receipt of a positive SARS-CoV-2 molecular or rapid antigen detection test result during hospitalization or during the 14 days preceding hospital admission. Demographic data were collected on all COVID-19–associated hospitalizations in 13 states and used to calculate age-stratified hospitalization rates.** Clinical data (signs and symptoms at admission,†† underlying medical conditions, and indicators of severe disease) were available for infants aged <6 months from 12 states.§§ Using previously described methods (4), clinical data were collected on all infant COVID-NET cases. Because of the surge in hospitalizations during December 2021 and January 2022, some sites abstracted clinical data on a representative sample of hospitalized infants.¶¶ A birth hospitalization was defined as the hospitalization during which the infant was born.
This analysis describes weekly COVID-19–associated hospitalization rates (hospitalizations per 100,000 population) and clinical characteristics of infants aged <6 months during June 20, 2021–August 31, 2022, which includes SARS-CoV-2 Delta (June 20–December 18, 2021), Omicron BA.1 (December 19, 2021–March 19, 2022), Omicron BA.2 (March 20–June 18, 2022), and Omicron BA.5 (June 19–August 31, 2022) variant–predominant periods. Hospitalization rates from the pre-Delta period and among all other age groups are included for comparison. Average weekly rates and demographic and clinical characteristics of infants aged <6 months were compared across variant-predominant periods. Unadjusted weekly COVID-19–associated hospitalization rates were calculated by dividing the total number of hospitalized patients by population estimates within each age group for the counties included in the surveillance catchment area.*** Because population estimates are available in 1-year age increments, population denominators for hospitalization rates among infants aged <6 months were calculated as one half the population estimate for infants aged <1 year. Three-week moving averages are presented for visualization purposes. Rate ratios (RRs) and 95% CIs were calculated. Demographic characteristics, clinical outcomes, and severity across SARS-CoV-2 variant-predominant periods were compared; the Omicron BA.2- and BA.5-predominant periods were combined in analyses because of small sample sizes. During the combined Omicron BA.2/BA.5-predominant period, the proportions of hospitalized infants with underlying medical conditions and symptoms on admission by age group (<1 month, 1–3 months, 4–5 months) were estimated. Wilcoxon rank-sum tests and chi-square tests were used to compare medians and proportions, respectively; p-values <0.05 were considered statistically significant. Percentages were weighted to account for the probability of selection for sampled cases, and further adjusted to account for nonresponse (i.e., an incomplete chart review). Data were analyzed using SAS (version 9.4; SAS Institute). This activity was reviewed by CDC and conducted consistent with applicable federal law and CDC policy.†††
During the Omicron BA.2/BA.5-predominant period, the weekly hospitalization rate among infants aged <6 months increased elevenfold (95% CI = 4.3–33.3) from a nadir of 2.2 (week ending April 9, 2022) to a peak of 26.0 (week ending July 23, 2022) and began to decline thereafter (Figure). The mean weekly hospitalization rate in this group was higher during the Omicron BA.2/BA.5 period (13.7) than during the Delta period (8.3) (RR = 1.6; 95% CI = 1.4–1.8). Compared with the Delta period, rates were also higher during the BA.2/BA.5 period among infants and children aged 6 months–4 years (RR = 1.9) and adults aged ≥75 years (RR = 1.4) but lower among children and adolescents aged 5–17 years (RR = 0.9), adults aged 18–64 years (RR = 0.5), and adults aged 65–74 years (RR = 0.8). The mean weekly hospitalization rate among infants aged <6 months during the Omicron BA.2/BA.5 period (13.7) was less than that of adults aged ≥75 years (39.4), similar to that of adults aged 65–74 years (13.8) and higher than rates in all other pediatric age groups (2.3 and 0.8 for children aged 6–23 months and 2–4 years, respectively) and in adults aged <65 years (4,6).
Complete clinical data were available for 1,116 infants aged <6 months hospitalized with laboratory-confirmed COVID-19, including 321, 322, and 473 infants hospitalized during the Delta, Omicron BA.1, and Omicron BA.2/BA.5 periods, respectively (Table 1). Differences during the three periods were small, and not all were statistically significant; however, indicators of severity, including length of hospital stay, and the proportion of hospitalizations that required intensive care unit admission, high-flow nasal cannula, mechanical ventilation, or bilevel positive airway pressure/continuous positive airway pressure (BiPAP/CPAP) were consistently lower during the Omicron BA.2/BA.5 period than during the Delta period, and in-hospital deaths were rare (<1%).
Among 473 infants aged <6 months hospitalized during the Omicron BA.2/BA.5 variant-predominant period, 397 (84%) had COVID-19–related symptoms. Among all 473 infants, 174 (38%) were aged <1 month; 69 (39%) of these were birth hospitalizations (Table 2). Among infants who received a positive SARS-CoV-2 test result during the birth hospitalization, 60 (87%) were asymptomatic. Excluding birth hospitalizations, similar proportions were hospitalized with COVID-19–related symptoms among infants aged <1 month (94%), 1–2 months (97%) and 3–5 months (96%). At least one underlying medical condition was present in 26% of hospitalized infants aged 1–2 months and 36% of those aged 3–5 months. Prematurity§§§ was the most frequently reported underlying condition (20% and 25% of infants aged 1–2 months and 3–5 months, respectively). Most infants aged 1–2 months (74%) and 3–5 months (68%) had fever on admission.
https://www.cdc.gov/mmwr/volumes/71/wr/mm7145a3.htm?s_cid=mm7145a3_w
Créditos: Comité científico Covid




