CONDENA MH CLÚSTER ATAQUE ARMADO A HOSPITAL ARCÁNGELES
Leer más
Tick-borne encephalitis (TBE)

Tick-borne encephalitis (TBE) virus is spread through the bite of an infected tick. Occasionally, TBE virus can spread to people through eating or drinking raw milk or cheese from infected goats, sheep, or cows.
TBE virus can be found in parts of the region stretching from western and northern Europe through northern and eastern Asia. People who travel to these areas might be at risk for infection. TBE virus is not found in the United States. The ticks that spread TBE virus are most active in warmer months (April through November). People who spend time outdoors in or near forests are at highest risk of being bitten by a tick infected with TBE virus.
Prevention
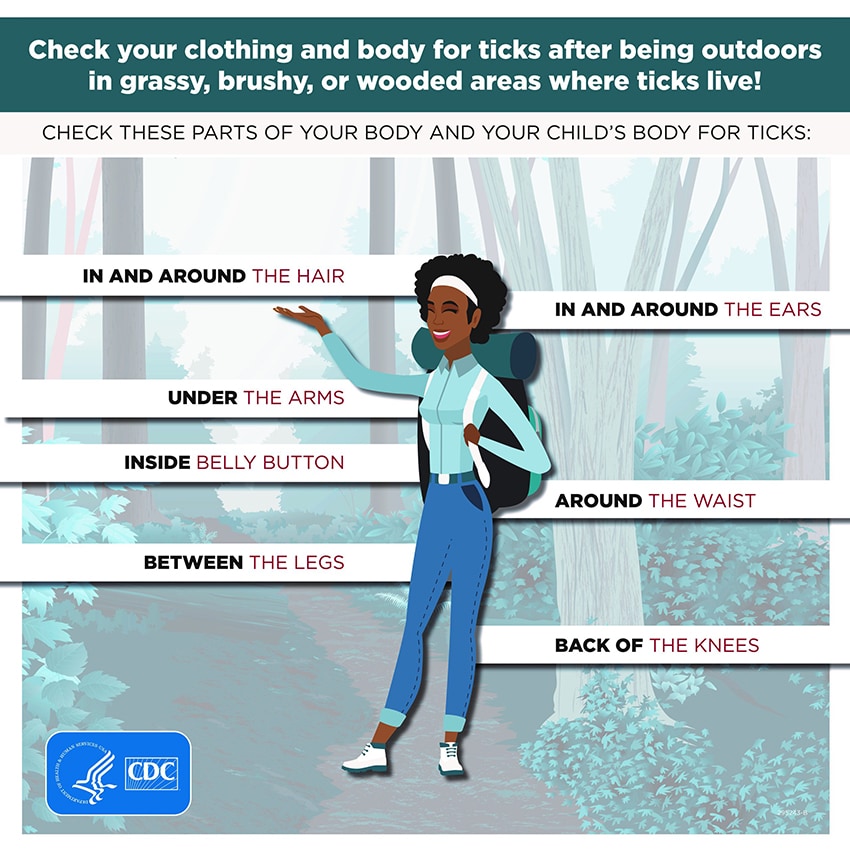
Tick-borne encephalitis (TBE) virus is most commonly spread to people through the bite of an infected tick. Ticks that spread TBE virus live in or near forests in parts of Europe and Asia. The best way to prevent TBE is to protect yourself from tick bites. Use insect repellent and treat clothing and gear with 0.5% permethrin. Inspect your body and clothing for ticks during and after outdoor activities.
To avoid getting TBE from infected dairy products, avoid eating or drinking unpasteurized (raw) milk and cheese from goats, sheep, or cows in affected areas.
Symptoms, Diagnosis, and Treatment
Symptoms
- Many people infected with tick-borne encephalitis (TBE) virus do not have symptoms.
- For people with symptoms, the time from tick bite to feeling sick is usually about 7 to 14 days, but can range from about 4 to 28 days.
- Severe disease often occurs including infection of the brain (encephalitis) or the membranes around the brain and spinal cord (meningitis).
- Initial symptoms can include fever, headache, vomiting, and weakness.
- A few days later, severe symptoms can develop including confusion, loss of coordination, difficulty speaking, weakness of the arms or legs, and seizures.
- Sometimes initial symptoms last a few days and completely resolve, but then about a week later the more severe symptoms develop (known as “biphasic illness”).
Diagnosis
- Healthcare providers diagnose TBE virus infection based on
- Signs and symptoms
- Travel history and possible exposure to ticks while traveling
- Laboratory testing of blood or spinal fluid
- More information on diagnostic testing is available here.
Treatment
- There is no medication to treat TBE virus infection.
- People with severe disease often need to be hospitalized to receive support for breathing, staying hydrated, or reducing swelling in the brain.
- If you think you or a family member might have TBE, see your healthcare provider.
- To learn more about treatment, visit our Healthcare Provider page.
-
Transmission

Ticks, specifically hard ticks of the family Ixodidae, transmit tick-borne encephalitis (TBE) virus. Ticks become infected when they feed on blood from infected vertebrate hosts, particularly small rodents, and can subsequently transmit the virus during the next blood meal. Ticks can also get the virus transtadially (from larva to nymph to adult ticks), transovarially (from adult female tick to eggs), or when cofeeding on infected animals. The highest period of tick activity and risk of spread is during the warmer months from April through November.
Infection also may follow consumption of unpasteurized milk or cheese from infected goats, sheep, or cows. Other rare modes of transmission include through slaughtering of infected animals, blood transfusion, organ transplantation, breastfeeding, or from exposure to the virus in the laboratory.
Vaccine
 resize iconView Larger
resize iconView LargerIn 2021, the U.S. Food and Drug Administration approved a tick-borne encephalitis (TBE) vaccine for use in the United States, called TICOVAC. This vaccine has been used for over 20 years in Europe. U.S. travelers visiting parts of Europe and Asia where TBE is found who might participate in outdoor activities with risk of tick exposure should talk to their healthcare provider about vaccination.
Who Should Get Vaccinated?
The risk for TBE is very low for most travelers visiting countries where TBE is found. However, travelers are at increased risk if they plan to:
- Visit areas with TBE when ticks are most active (April through November)
- Take part in outdoor activities in or near forested areas such as hiking, camping, hunting, fishing, or birdwatching.
All travelers visiting countries with TBE should take steps to avoid tick bites. If you plan to travel during the warmer months of the year and participate in outdoor activities, you should discuss the need for vaccination with your healthcare provider. When discussing whether or not to be vaccinated against TBE, consider the following:
- What locations you will be visiting
- What activities you will participate in while traveling
- Likelihood of future travel to countries where TBE is found
- Potential severe outcomes of TBE disease
- Vaccine doses, cost, and possible side effects
The TBE vaccine is available for children aged 1 year and older and adults. Three doses are needed to complete the series so you should talk to your healthcare provider as early as possible before travel.
For more information, please visit our healthcare provider page.
Créditos: Comité científico Covid




