CONDENA MH CLÚSTER ATAQUE ARMADO A HOSPITAL ARCÁNGELES
Leer más
Vitamin D Deficiency and Related Disorders
Practice Essentials
Vitamin D deficiency can result from inadequate exposure to sunlight; malabsorption; accelerated catabolism from certain medications; and, in infants, the minimal amount of vitamin D found in breast milk. In children, vitamin D deficiency can result in rickets, which presents as bowing of the legs; in adults, it results in osteomalacia, which presents as a poorly mineralized skeletal matrix. See the image below.
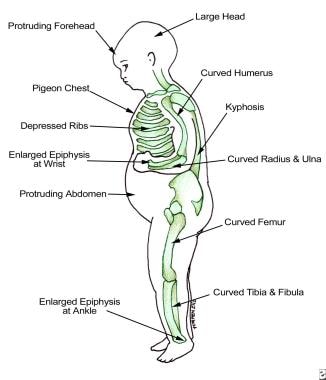 Findings in patients with rickets.
Findings in patients with rickets.
Signs and symptoms
Vitamin D deficiency is often clinically silent. Manifestations are as follows:
-
Children are often found to have started walking late or prefer to sit down for prolonged periods
-
Adults can experience chronic muscle aches and pains
Physical findings in severe vitamin D deficiency are as follows:
-
In children, bowing in the legs
-
In adults, periosteal bone pain, best detected with firm pressure on the sternum or tibia
See Clinical Presentation for more detail.
Diagnosis
Measurement of serum 25-hydroxyvitamin D (25[OH]D) is the best test to determine vitamin D status. Levels of 25(OH)D are interpreted as follows [1] :
-
21-29 ng/mL (52.5-72.5 nmol/L): Vitamin D insufficiency
-
< 20 ng/mL (< 50 nmol/L): Vitamin D deficiency
Although not always required for the diagnosis of vitamin D insufficiency, measurement of the serum parathyroid hormone (PTH) level may help establish the diagnosis of vitamin D insufficiency. PTH levels are often elevated in patients with vitamin D insufficiency, indicating secondary hyperparathyroidism.
Screening for vitamin D deficiency is recommended only in those individuals who are at high risk for vitamin D deficiency, including the following [2] :
-
Patients with osteoporosis
-
Patients with a malabsorption syndrome
-
Black and Hispanic individuals
-
Obese persons (body mass index >30 kg/m2) [3]
-
Patients with disorders that affect the metabolism of vitamin D and phosphate (eg, chronic kidney disease)
See Workup for more detail.
Management
Recommended treatment for vitamin D–deficient patients up to 1 year of age is as follows [2] :
-
2000 IU/day of vitamin D2 or D3 for 6 weeks or
-
50,000 IU of vitamin D2 or D3 once weekly for 6 weeks
-
When the serum 25(OH)D level exceeds 30 ng/mL, provide maintenance treatment of 400-1000 IU/day
Recommended treatment for vitamin D–deficient patients 1–18 years of age is as follows [2] :
-
2000 IU/day of vitamin D2 or D3 for at least 6 weeks or
-
50,000 IU of vitamin D2 once weekly for at least 6 weeks
-
When the serum 25(OH)D level exceeds 30 ng/mL, provide maintenance treatment of 600-1000 IU/day
Recommended treatment for vitamin D–deficient adults is as follows [2] :
-
50,000 IU of vitamin D2 or D3 once weekly for 8 weeks or
-
6000 IU/day of vitamin D2 or D3 for 8 weeks
-
When the serum 25(OH)D level exceeds 30 ng/mL, provide maintenance treatment of 1500-2000 IU/day
Recommended treatment for vitamin D–deficient patients who are obese, have a malabsorption syndrome, or are taking medication that affects vitamin D metabolism, is as follows [2] :
-
At least 6000-10,000 IU of vitamin D daily
-
When the serum 25(OH)D level exceeds 30 ng/mL, provide maintenance treatment of 3000-6000 IU/day
If the 25(OH)D concentration remains persistently low despite several attempts at correction with oral vitamin D, a trial of ultraviolet B light therapy (ie, by tanning lamps) may be considered to improve vitamin D status.
Prevention
Unprotected sun exposure is the major source of vitamin D for both children and adults. [2] Provision of vitamin D from sunlight is as follows:
-
Sensible sun exposure, especially between the hours of 10 am and 3 pm, produces vitamin D in the skin that may last twice as long in the blood compared with ingested vitamin D [4]
-
Full-body sun exposure producing slight pinkness in light-skinned persons results in vitamin D production equivalent to ingesting 10,000-25,000 IU [5]
-
Increased skin pigmentation, aging, and sunscreen use reduce the skin’s vitamin D3 production
Recommended dietary intake of vitamin D for patients at risk of vitamin D deficiency is as follows [2] :
-
In infants and children up to 1 year old, at least 400 IU/day, to maximize bone health
-
In children and adolescents 1-18 years of age, at least 600 IU/day to maximize bone health
-
In adults 19-50 years of age, at least 600 IU/day to maximize bone health and muscle function
-
Raising the serum 25(OH)D level consistently above 30 ng/mL may require vitamin D intake of at least 1000 IU/day
-
Whether recommended levels of vitamin D intake will provide all the potential nonskeletal health benefits associated with vitamin D is currently unknown
Most dietary sources of vitamin D do not contain sufficient amounts of the vitamin to satisfy daily requirements. The following foods contain the indicated amounts of vitamin D, as reported by the US Department of Agriculture’s (USDA’s) Nutrient Data Laboratory:
-
Fortified milk (8 oz) – 100 IU
-
Fortified orange juice (8 oz) [6] – 100 IU
-
Fortified cereal (1 serving) – 40-80 IU
-
Pickled herring (100 g) – 680 IU
-
Canned salmon with bones (100 g) – 624 IU
-
Mackerel (100 g) – 360 IU
-
Canned sardines (100 g) – 272 IU
-
Codfish (100 g) – 44 IU
-
Swiss cheese (100 g) – 44 IU
-
Raw shiitake mushrooms (100 g) – 76 IU
-
Most multivitamins (1 tab) – 400 IU
See Treatment and Medication for more detail.
Créditos: Comité científico Covid




