CONDENA MH CLÚSTER ATAQUE ARMADO A HOSPITAL ARCÁNGELES
Leer más
Efficacy, Immunogenicity and Safety of COVID-19 Vaccines: A Systematic Review and Meta-Analysis
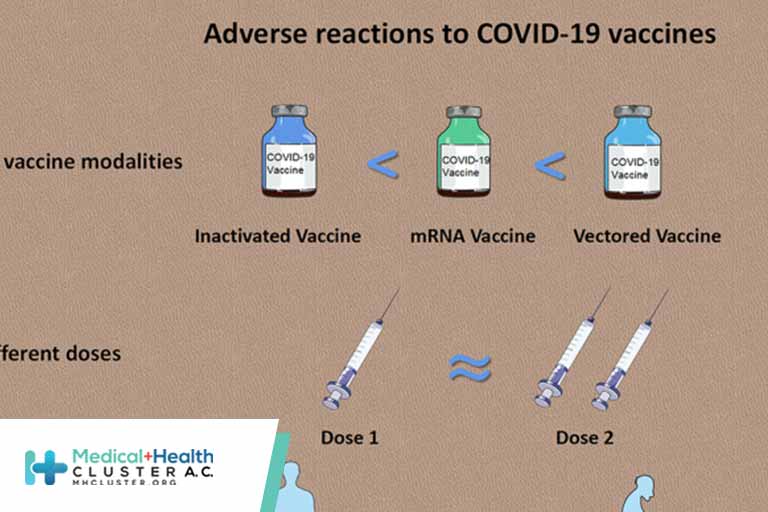
There is a significant research gap in meta-analysis on the efficacy and safety of coronavirus disease 2019 (COVID-19) vaccines. This study analyzed the efficacy of COVID-19 vaccines. Published phase I, phase II, and phase III trials analyzing safety and immunogenicity and phase III randomized clinical trials evaluating the efficacy of COVID-19 vaccines were included. We searched MEDLINE, Scopus, and The Lancet for published articles evaluating the relative reduction in COVID-19 risk after vaccination. Selected literatures were published between December 15, 2019 and May 15, 2021 on the safety, efficacy, and immunogenicity of COVID-19 vaccines. This meta-analysis included studies that confirmed cases of COVID-19 using reverse transcriptase polymerase chain reaction. This study detected 8,926 eligible research articles published on COVID-19 vaccines. Of these, 25 studies fulfilled the inclusion criteria. Among the selected articles, 19 randomized clinical trials, 2 non-randomized clinical trials, and 3 observational studies were analyzed. Seven (28%) studies were included in the meta-analysis. The efficacy of the adenovirus vector vaccine was 73% (95% CI = 69–77) and that of the messenger RNA (mRNA) vaccine was 85% (95% CI = 82–88) in participants aged ≥18 years. There are no reports of clinical trials in participants aged under 16 years. The production of neutralizing antibodies against receptor-binding domains (RBDs) of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in >90% of the vaccinated samples was reported within 0–30 days of the first or the second dose of the vaccine. Pain at the injection site was the most common local symptom in people receiving mRNA vaccines (29%–85% of participants). Fever (0.2%–95%) was the most prevalent in people receiving adenovirus vector vaccines, and fatigue (8.4%–55%) was the most common side effect in people receiving the mRNA vaccines. Studies suggest that mRNA vaccines and adenovirus vector vaccines can provide moderate to high protection against COVID-19 infection in people over 18 years. Evidence of the long-term protection of the vaccines in people aged under 16 years against the multiple variants of COVID-19 are limited. This study will provide an integrated evaluation on the efficacy, safety, and immunogenicity of the COVID-19 vaccines.
Introduction
A novel species of coronavirus, namely, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has set out the coronavirus disease 2019 (COVID-19) pandemic from December 2020 (1). About 150 million cases and 3.2 million fatalities associated with COVID-19 have been confirmed globally (2, 3). The odds of acquiring health issues are higher in the elderly, healthcare workers, persons with comorbidities, and those who live in areas with high community transmission (4–8). According to recent studies, children and younger adults are also becoming infected with COVID-19 and are having serious health problems (4). The majority of the world’s population is still uninfected. However, the number of illnesses and fatalities are continuously increasing (2, 3). If adequate preventive actions are not performed quickly, COVID-19 will have serious and long-term medical, social, economic, and mental effects (9, 10).Effective vaccines are one of the most significant preventive measures to contain infectious diseases (10). Immunization against COVID-19 via vaccines will not only prevent the spread of the virus but will also limit the serious health consequences of the pandemic (9, 10). Several vaccine candidates have been tested and found to be effective and safe against COVID-19. Since December 2020, different countries have begun mass vaccinations and targeted population vaccinations. Two messenger RNA (mRNA) vaccines, three adenovirus vector vaccines, four inactivated vaccines, and two protein subunit vaccines have been approved for use against COVID-19 at the national and international levels (9, 11, 12). The safety and efficacy of these vaccine candidates were evaluated in laboratory studies, randomized clinical trials, and observational studies before they were approved for emergency or full use (9, 10).Vaccines against COVID-19 were developed and utilized in a relatively short period of time compared to other vaccines. As a result, the efficacy, safety, and side effects of the vaccines against COVID-19 require continuous and extensive surveillance and research (9, 10). Three factors should be considered to assess the effectiveness and safety of the COVID-19 vaccines for long-term prevention: the emergence of new SARS-CoV-2 variants with altered infection capacity and immune neutralization properties, the side effects of the vaccine in different socio-demographic settings, and the longevity of the produced antibodies against the virus (9, 10, 13–15). New variants, namely, alpha (B.1.1.7), beta (B.1.351), gamma (P.1), iota (B.1.526), epsilon (B.1.429), and delta (B.1.617.2), have emerged and have been transmitted to different countries within short periods of time (14, 15). As a result, randomized controlled trials and observational studies are needed to confirm the efficacy of the existing vaccines against the newly emerged variants (13, 15).One of the most important predictors of vaccine acceptance in recipients is the safety of the available vaccines (16–20). In the majority of randomized clinical and observational studies, local and systematic reactions in recipients after vaccination have been reported in the mRNA vaccines, adenovirus vector vaccines, inactivated virus vaccines, and the protein subunit vaccines (16, 17, 21–26). Both single-dose and double-dose vaccines had side effects.The most common local reactions were pain, erythema, swelling, and lymphadenopathy at the injection site, while headache, fatigue, myalgia, and nausea were the most common systemic side effects of the COVID-19 vaccines (27–35). Serious grade 3 consequences possibly associated with COVID-19 were detected at a very low frequency among participants in an adenovirus vaccine clinical trial. In terms of immunogenicity, the majority of studies found that the approved vaccines were effective in stimulating the production of neutralizing antibodies against the receptor-binding domains (RBDs) of SARS-CoV-2 (18, 21–24, 28, 29, 36). However, more studies are needed to assess the persistence of immunity after vaccination. There are currently no published systematic reviews or meta-analyses that integrate and evaluate the efficacy and safety of all COVID-19 vaccines. The main aim of this study was to investigate the published literatures in order to evaluate the efficacy, immunogenicity, and safety of the COVID-19 vaccines.
Methods
Definitions and Outcomes
The efficacy of a COVID-19 vaccine was defined as the relative reduction in SARS-CoV-2 infection risk following vaccination, as determined by previously published randomized placebo-controlled clinical trials (26, 30, 32, 37). The safety of a COVID-19 vaccine was determined in this study as the health outcome after vaccination under acceptable conditions, as defined by previously published research. This study included both observational, randomized and non-randomized controlled studies. Positive reverse transcriptase PCR (RT-PCR) results for COVID-19 were considered as laboratory-confirmed cases. Published observational studies and randomized and non-randomized controlled trials were selected based on the inclusion criteria. Efficacy was considered statistically significant when the 95% CI for efficacy did not cross 0 for all studies. The reporting of this systematic review was guided by the standards of the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statement (38).
Search Strategy and Selection Criteria
Different electronic websites, databases, and journals, including MEDLINE (through PubMed), EMBASE, Web of Science, Scopus, The Lancet, and The New England Journal of Medicine (NEJM), were searched to detect published articles on the efficacy and safety of the COVID-19 vaccines from December 15, 2019 to May 15, 2021. Preprint repositories such as medRxiv, bioRxiv, SSRN, and AAS Open Research were also searched for related preprint articles. Additionally, the first 20 pages of the Google Scholar search engine were manually screened for relevant articles. The language of the articles that were reviewed was limited to English. This study used the following combinations as search terms: COVID-19, SARS‐CoV‐2, vaccine, safety, efficacy, side effects, effectiveness, clinical trial, observational study, randomized controlled study, mRNA vaccine, adenovirus vector vaccine, subunit vaccine, inactivated vaccine, variants, B.1.1.7, B.1.351, P.1, B.1.526, B.1.429, B.1.617, alpha, beta, gamma, delta, iota, epsilon, China, the USA, the UK, India, Russia, Australia, Brazil, ChAdOx1 nCoV-19, Ad26.COV2.S, mRNA-1273, BNT162b1, BNT162b2, rAd26, rAd5, and MF59-adjuvanted spike glycoprotein-clamp.As this is an early meat-data analysis based on the available studies published within the last 2 years, it included studies on any strain of SARS-CoV-2. NS and SD evaluated the eligible studies. All included studies were evaluated for quality by NS, KA, and SA. The risk of bias was studied using The Systematic Review Centre for Laboratory Animal Experimentation (SYRCLE) assessment tool (39). The evaluation of SYRCLE consisted of 10 parameters to assess various biases, including attrition bias, selection bias, detection bias, reporting bias, performance bias, and other biases. The measurement of bias was done using possible outcomes for each parameter as yes, no, and unclear, indicating low, high, and unclear risk of bias, respectively (39).This review excluded studies on the acceptance and challenges of the COVID-19 vaccines, which were not related to natural infection and were not comparable to other studies. The exclusion criteria were as follows: studies that only reported nonspecific outcomes, such as a reduction in the period of illness, mortality, or COVID-19-like illness; studies that did not provide efficacy or safety or immunogenicity data for the COVID-19 vaccines; and non-comparable parallel studies with unspecific clinical outcomes, as unspecific outcomes could lead to unmeasured confounding and complicate the interpretation.We could not implement seasonal exclusion criteria due to the lack of seasonal studies. We could not also rule out studies that did not report specific variant properties due to lack of data. Safety and side effect studies based on self-reporting were excluded. Safety studies were excluded unless they used systematic sampling of participants using well-defined symptom criteria.
Inclusion Criteria for Efficacy Studies
Randomized controlled trials published in peer-reviewed journals indexed by PubMed were included in this analysis. Studies with large numbers of participants in which the outcomes were defined as RT-PCR-confirmed cases by following standard guidelines of the WHO were included in this article. We also included studies where the control group received a placebo or a vaccine other than SARS-CoV-2 and studies where the concentrations of the mRNA vaccines were presented in microgram amounts and the adenovirus vector vaccines in 1010–1011 virus particles.
Inclusion Criteria for Safety and Immunogenicity Studies
This work included articles that published phase I/phase II/phase III clinical trials of the COVID-19 vaccines in peer-reviewed journals indexed by PubMed. We included studies that measured the severity of the side effects of the COVID-19 vaccines using the WHO guidelines; studies reporting the production of neutralizing antibodies against RBDs within 0–30 days of vaccination; studies reporting the immunogenicity of both the first and second doses of the vaccine; studies in which the control group received placebo or vaccines other than SARS-CoV-2; and studies in which the side effects were monitored and evaluated by experts. Summary data were extracted from published works for all of the studies.
Statistical Analysis
This study used the Mantel–Haenszel fixed effects method (random effects pooled odds ratios with 95% CI) for three or more randomized controlled trials on similar COVID-19 vaccines. The Breslow–Day statistic was used to assess the homogeneity of the odds ratios. Vaccine efficacy was calculated using the random effects odds ratio. This study applied the accepted statistical vaccine efficacy formula, (1 − odds ratio) × 100, for calculating the pooled odds ratios to establish pooled vaccine efficacy. This study interpreted the protective efficacy point of the vaccine and the CI. We included negative estimations as zero efficacy. Statistical analyses were conducted using SAS version 9.4.
Créditos: Comité científico Covid




